Ductal Carcinoma In Situ (DCIS)
Breast cancer is caused by cells in the breast that grow out of control. As the number of cells grow, they form a mass (tumor). Ductal carcinoma in situ (DCIS- also known as intraductal carcinoma) is the earliest form of breast cancer and is sometimes called “stage 0” breast cancer. About 1 in 5 breast cancers are DCIS.
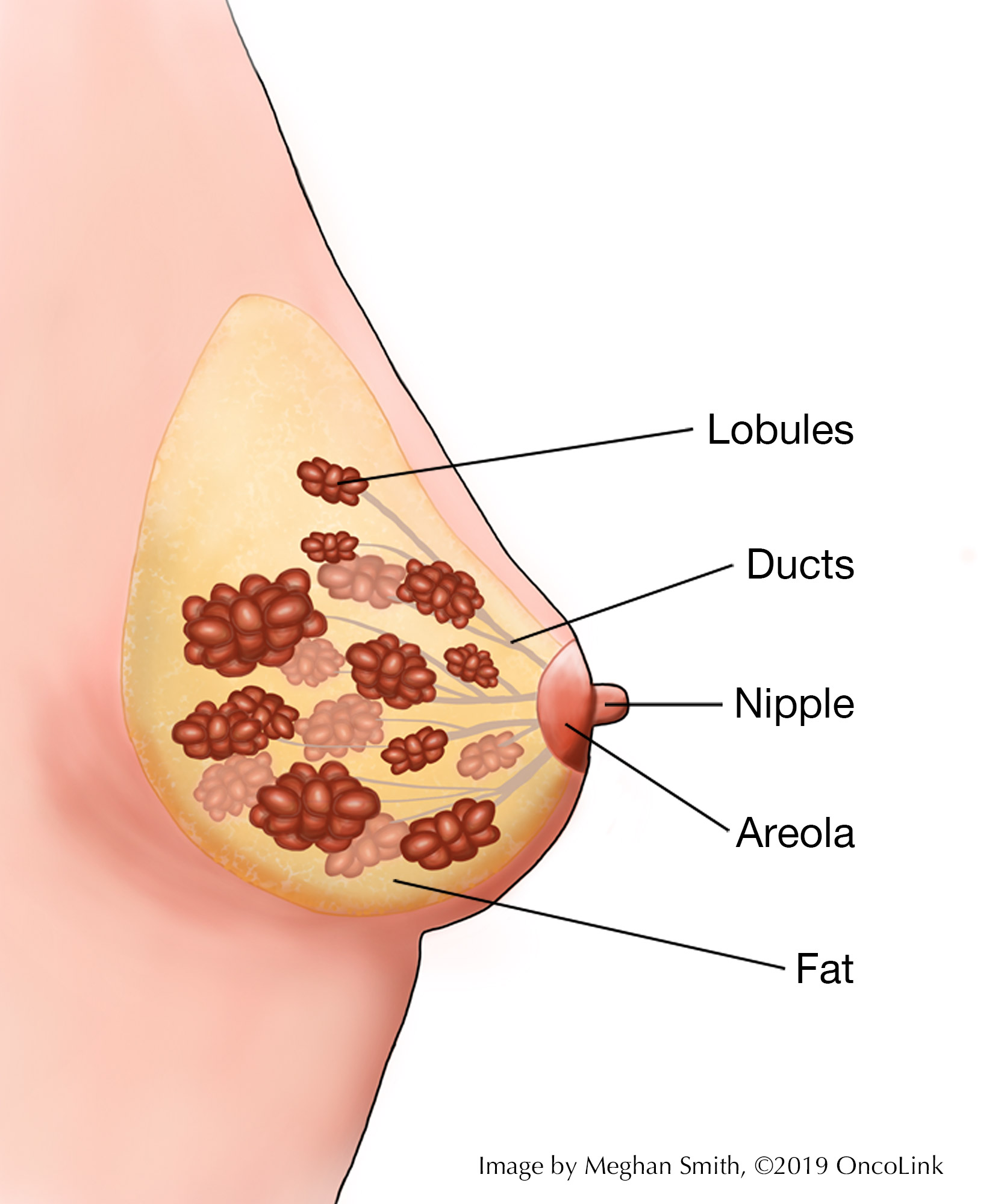
What makes up the breast tissue?
Breast tissue is made up of lobules, which make milk, and ducts, which carry the milk to the nipple. Lobules and ducts are made up of glandular tissue. Glandular tissue helps secrete hormones in the body. Almost all breast cancers start in glandular tissue. These cancers are called adenocarcinomas (cancer of the glandular tissue). Breast cancer starts in a duct or a lobule and this, along with how it looks under the microscope, determines the type of breast cancer it is.
What is DCIS?
DCIS happens when the cells that line the ducts of the breast have changed to cancer cells but are “noninvasive” or “pre-invasive.” This means they have not spread past the lining of the duct into nearby breast tissue. The cancer cells are only in the milk duct where they started. The cells in DCIS are malignant (cancerous), and as they grow, the center of the tumor starts to die because it has outgrown its blood supply. This area of dead tissue, called necrosis, can calcify (harden).
How is DCIS diagnosed?
A mammogram is an x-ray picture of the breast. Most often, DCIS is found on a mammogram that is used to screen for breast cancer. In rare cases, you may feel a lump in the breast or have bloody discharge from the nipple. Your healthcare provider would send you for a mammogram or ultrasound to figure out the cause of these symptoms.
If the radiologist sees something on the mammogram that needs to be looked at more, you may need more tests done. These can include repeat mammogram pictures, ultrasound, or biopsy to test the breast tissue. A biopsy is used to diagnose DCIS.
After the biopsy, the tissue sample is looked at by a pathologist under a microscope and a report is written. A pathologist is a medical doctor who specializes in diagnosing diseases by looking at tissue taken from the body. The pathology report gives information about you and your health history, the reason for the test, and both normal and abnormal findings. The classification of your tumor will also be in the report. These things are discussed below. You should ask for a copy of the pathology report for your records.
How is DCIS classified?
DCIS can be classified by grade and how the cells look under the microscope, as well as hormone-receptor status. Classification can help determine treatment options.
Grade
DCIS can be classified by grade. The lower the grade, the more the cancer cells look like normal breast cells. Lower grades also tend to grow more slowly. Sometimes the cells might be a mix of grades, which may be called “borderline” cells. The grades of DCIS are:
- Grade I (low grade, or nuclear grade I)- The cancer cells look a lot like normal breast cells under a microscope.
- Grade II (moderate grade, or nuclear grade 2)- These cells grow faster than normal breast cells and look a little less like the normal cells.
- Grade III (high grade, or nuclear grade 3)- These cells grow faster and look much different than normal breast cells. People with high-grade cancers have a higher chance of developing invasive breast cancer in the future or having the current cancer come back after treatment.
Appearance
DCIS cells are further identified by their pattern or shape when looked at under the microscope, classifying them into subtypes. Many tumors will be a mix of two or more subtypes. These subtypes are:
Low or Moderate Grade:
- Papillary- The cancer cells in the duct look finger-like.
- Micropapillary- A type of papillary where the cells are very small.
- Cribiform- Spaces or gaps are seen between the cancer cells in the duct.
- Solid- There is a solid collection of cancer cells without spaces between them.
High Grade:
- Comedo- There is a solid collection of cancer cells, with an area in the middle that is made up of dead cells (also called necrotic). The cancer cells build up quickly within the duct and some cells inside the tumor lose their blood supply, causing necrosis.
Hormone Status
Your provider may test your cells for hormone receptors. If there are receptors for estrogen and/or progesterone (hormones) found on the cancer cells, the tumor is called hormone receptor-positive (ER+/PR+, ER+/PR- or ER-/PR+). When estrogen or progesterone attaches to the receptor, it lets the cancer cell grow and divide. Hormone receptor status (positive or negative) is used to pick which treatments you may receive. Hormone therapy can be used to block these receptors, by slowing or stopping tumor growth or preventing recurrence (cancer coming back).
You may have heard a friend or family member talk about "HER2" positive or negative. The status of HER2 in DCIS does not guide treatment options, so your provider will likely not test for HER2.
How is DCIS treated?
DCIS can become an invasive cancer, or one that spreads to other areas. Once it has spread outside of the duct and into nearby tissue, it can then spread to other parts of the body (metastasize) and can be harder to treat. There is no way to tell if DCIS will become an invasive cancer, so almost all cases of DCIS are treated. Some treatment options for DCIS are:
- Lumpectomy, With or Without Radiation Therapy: This is the most common treatment for DCIS. A lumpectomy (also called breast-conserving surgery) is removal of only the breast mass/tumor, and not the whole breast. The mass is removed, along with a small area of surrounding normal breast tissue. After this surgery, you may have radiation therapy. Radiation therapy uses high energy x-rays to damage the DNA of cells. This kills the cancer cells or stops them from reproducing and lowers the risk that the cancer will come back.
- Simple Mastectomy: A simple mastectomy is removal of the entire breast. This includes the nipple, skin, areola, and breast tissue. This might be needed if the area of DCIS is very big, if there are many ducts that have cancer cells, or if there are still cancer cells left in the breast after a lumpectomy.
- Sentinel Lymph Node Biopsy: Your provider may want to test your lymph nodes during a lumpectomy or mastectomy. The surgeon injects dye into the area of the tumor. The lymphatic system picks up the dye and takes it to nearby lymph nodes. An incision (cut) is made, and the surgeon finds the lymph nodes with dye in them. The nodes that pick up the dye are the sentinel lymph nodes. They are removed and tested for cancer cells.
- Hormone Therapy: If your biopsy shows that your DCIS is hormone-receptor positive, you may be treated with a medication called tamoxifen. If you are in menopause, an aromatase inhibitor medication may be given. Whichever type of medication is used, you will often take it for 5 years after a lumpectomy or mastectomy to lower the risk of the cancer from coming back or a new cancer developing.
- Clinical Trials: You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Service.
Making Treatment Decisions
Your care team will make sure you are included in choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It feels like an emergency, but you can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot make the decision for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
You can learn more about breast cancer at OncoLink.org.
References
American Cancer Society. (2019). Ductal Carcinoma In Situ (DCIS). Retrieved from https://www.cancer.org/cancer/breast-cancer/understanding-a-breast-cancer-diagnosis/types-of-breast-cancer/dcis.html.
American Cancer Society. (2019). Treatment of Ductal Carcinoma in Situ (DCIS). Retrieved from https://www.cancer.org/cancer/breast-cancer/treatment/treatment-of-breast-cancer-by-stage/treatment-of-ductal-carcinoma-in-situ-dcis.html.
Collins, L.C., Laronga, C., Wong, J.S. (2020). Ductal carcinoma in situ: Treatment and prognosis. Retrieved from https://www.uptodate.com/contents/ductal-carcinoma-in-situ-treatment-and-prognosis?search=dcis&source=search_result&selectedTitle=1~54&usage_type=default&display_rank=1.
National Institutes of Health: National Cancer Institue. (2015). Surgery Choices for Women with DCIS or Breast Cancer. Retrieved from https://www.cancer.gov/types/breast/surgery-choices.