Surgical Procedures: Vulvectomy
What is a vulvectomy and how is it done?
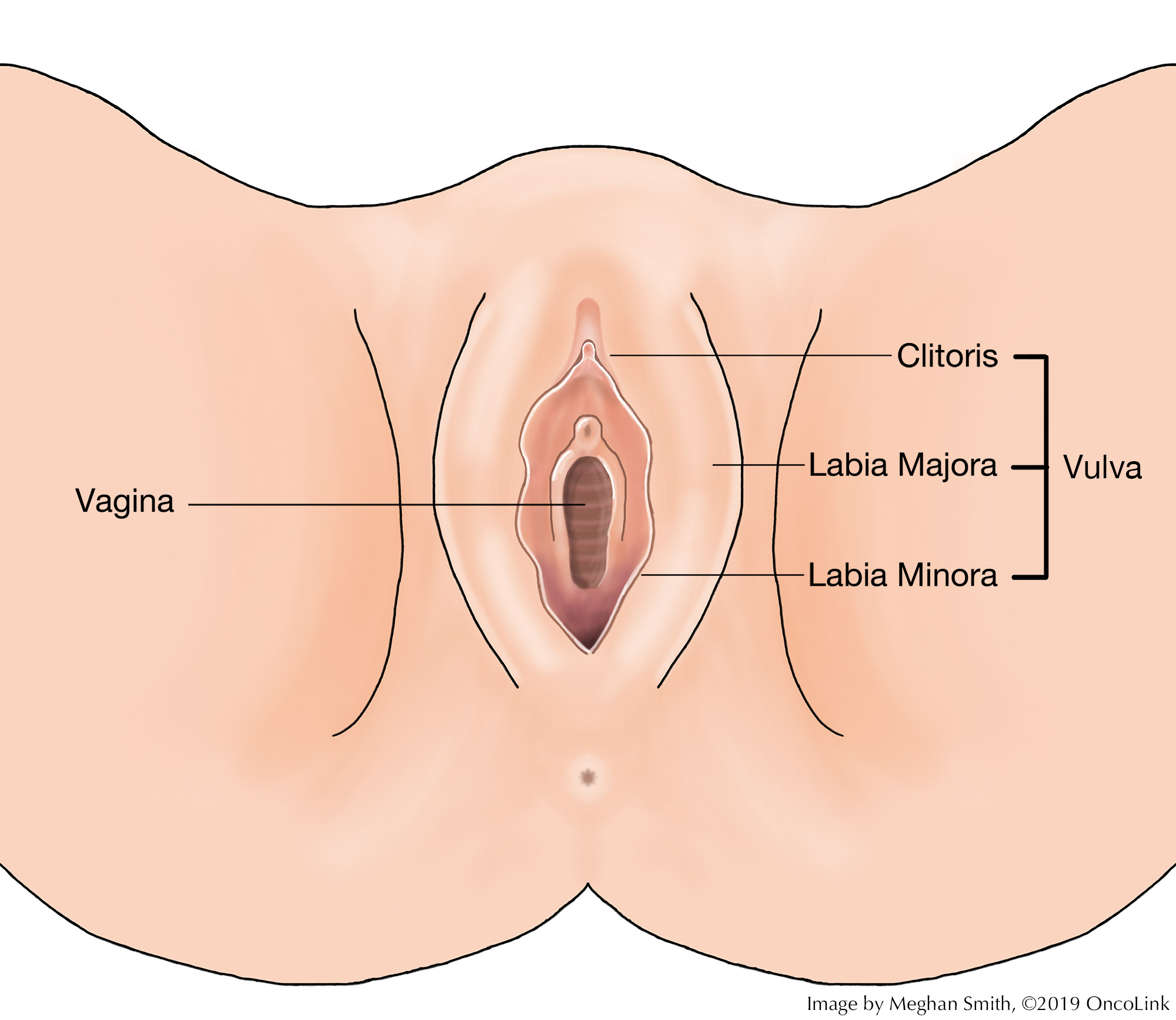
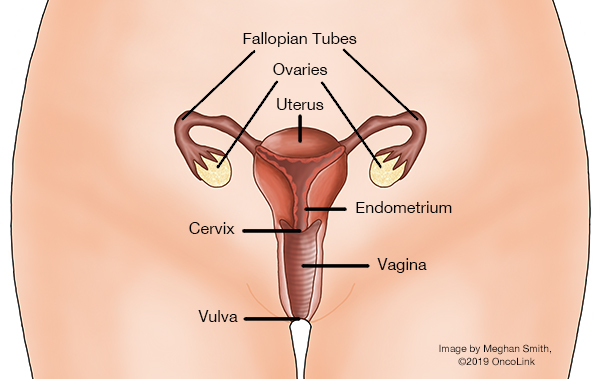
A vulvectomy is surgery to remove part of or all of the vulva. The vulva is the outer part of a woman’s genitals and includes:
- The labia minora and majora (small and large lips).
- Clitoris.
- Vestibule.
- Introitus.
- Urethral meatus.
- Glands and ducts.
Vulvectomy can be used to treat some cases of vulvar cancer.
The types of vulvectomy are:
- Skinning Vulvectomy: The top layer of the vulvar skin is removed.
- Simple Vulvectomy: The whole vulva is removed. The clitoris may also need to be removed.
- Modified Radical Vulvectomy: The vulva and some nearby lymph nodes and tissue are removed.
- Radical Vulvectomy: The whole vulva, many nearby lymph nodes, and tissue are removed.
After surgery, drains may be placed to remove fluid build-up from the surgical area. These are temporary (short-term) and will be removed in your provider’s office. You will be taught how to care for the drains. If needed, a home care nurse will come to help you.
Depending on the type of vulvectomy you had, you may need a skin graft. A skin graft is when an area of healthy tissue from another part of your body is removed. This piece of skin is then stitched into the areas of the vulva that need to be covered. For women who have had an extensive vulvectomy, reconstructive surgery is an option.
What are the risks and side effects of having a vulvectomy?
There are risks and side effects related to having a vulvectomy. Risks and side effects may be:
- Bleeding, infection and/or blood clots.
- Wound issues, such as delayed healing, infections, and graft site failure. Fluid-filled cysts can form under and near the wound.
- Urinary tract infections (UTI).
- Lymphedema (swelling) of the legs.
- Change in how the vulva looks, decreased libido (sex drive), genital numbness (may be short-term).
- Narrowed (thinner) vaginal opening, decreased sexual pleasure and/or painful intercourse.
- Discomfort and fatigue.
- Change in urine stream.
What is recovery like?
You may need to stay in the hospital for a few days after your procedure. A catheter may be placed to drain your bladder of urine.
You will be taught how to clean and dry your genitals. You will need to be careful drying your genitals. You will also be taught how to use a Sitz bath which is a shallow bath where you can place warm water. It is used to clean your genital area and help with pain and itching. Your provider will teach you how to do this. If you have dressings or bandages, they will be looked at daily and removed when needed.
Your care team will talk with you about the medications you will be taking, such as those for pain, blood clot, infection, and constipation prevention and/or other conditions.
What will I need at home?
- Soft, clean towels for cleaning and drying yourself.
- Sitz bath and a squirt bottle for vulvar hygiene, which is often given to you before leaving the hospital.
- Hair dryer with a cool setting or a circulating fan to dry the surgical area.
- Thermometer to check for fever, which can be a sign of infection. Your care team will tell you at what temperature you should call them.
- Loose clothing and cotton underwear.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.
OncoLink is designed for educational purposes only and is not engaged in rendering medical advice or professional services. The information provided through OncoLink should not be used for diagnosing or treating a health problem or a disease. It is not a substitute for professional care. If you have or suspect you may have a health problem or have questions or concerns about the medication that you have been prescribed, you should consult your health care provider.
Information Provided By: www.oncolink.org | © 2025 Trustees of The University of Pennsylvania