Surgical Procedures: Surgical Staging for Endometrial Cancer
The stage of your cancer tells how extensive the cancer is, if and how far it has spread, and what treatment may be best for you. Endometrial cancer can spread to other parts of the body through the lymph and blood systems. There are two systems to stage endometrial cancer:
- The FIGO staging system (International Federation of Gynecology and Obstetrics).
- The American Joint Committee on Cancer TNM staging system.
Both staging systems use the letters TNM to describe the cancer:
- T: The size and how far the tumor has grown into the uterus.
- N: Which, if any, lymph nodes have cancer in them.
- M: If it has spread (metastasis) to more distant areas of the body.
Terms such as local, regional, or distant metastasis may be used to describe the cancer.
- Local metastasis: The cancer has spread to the cervix and other areas of the uterus.
- Regional metastasis: The cancer has spread to lymph nodes that are nearby in the pelvis and along the aorta (para-aortic lymph nodes).
- Distant metastasis: The cancer has spread to distant lymph nodes, upper abdomen (belly), omentum (fatty tissue covering the abdominal organs), and to organs like the lung, liver, bone, and/or brain.
To learn more about staging of endometrial cancer, check out “Endometrial (Uterine) Cancer: Staging and Treatment.”
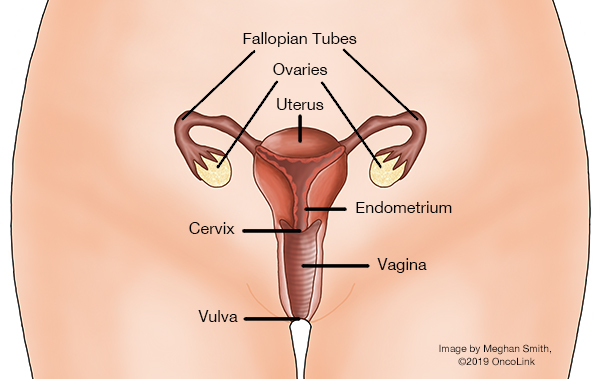
Women with stage I-III endometrial cancer will most likely need surgery. A hysterectomy is often recommended. A hysterectomy will cause infertility (being unable to get pregnant), so talk with your provider about any questions or concerns you may have.
There are many types of hysterectomy:
- Total Hysterectomy: The uterus and cervix are removed. The ovaries may be removed.
- Radical Hysterectomy: The uterus, cervix, tissue near the cervix, and the upper part of the vagina are removed. The fallopian tubes, ovaries, and lymph nodes may also be removed.
- Bilateral Salpingo-oophorectomy (BSO): The ovary and fallopian tube are removed. During a bilateral procedure, both the left and right ovary and tube are removed. A unilateral procedure only removes one side.
A hysterectomy can be done in different ways:
- Abdominal: An incision (surgical cut) is made in the abdomen to remove the uterus.
- Vaginal: An incision is made in the upper vagina.
- Laparoscopic: A laparoscope (a lighted tube with a camera) is used to see the pelvic organs. Small incisions are made in the abdomen where the tools are inserted.
- Robotic: The surgeon controls a robotic arm to perform the surgery through small incisions.
Lymph nodes may also be removed. Your treatment plan may also include chemotherapy and/or radiation therapy. Your provider will talk with you about if you may receive chemotherapy and/or radiation.
What does debulking mean?
If cancer has spread throughout your abdomen, your surgeon will try to remove as much of the tumor as possible. This is called “debulking.” Debulking is done to lessen the amount of cancer before starting radiation or chemotherapy.
What is recovery like?
Recovery from surgery for endometrial cancer will include a stay in the hospital. How long you are there depends on the type of hysterectomy you have had. You may have a bladder catheter in place for one to two days to drain your bladder of urine. You may need to go home with the catheter in place. You may have a home or visiting nurse to help with your catheter.
Take your prescribed medications as directed to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms. There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. Your healthcare provider will talk with you about when you can do activities like bathing, lifting, bending, going back to work, or having sex.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.
OncoLink is designed for educational purposes only and is not engaged in rendering medical advice or professional services. The information provided through OncoLink should not be used for diagnosing or treating a health problem or a disease. It is not a substitute for professional care. If you have or suspect you may have a health problem or have questions or concerns about the medication that you have been prescribed, you should consult your health care provider.
Information Provided By: www.oncolink.org | © 2025 Trustees of The University of Pennsylvania