Understanding Your Pathology Report: Breast Cancer
What is a pathology report?
A pathologist is a doctor who uses laboratory tests and techniques to help diagnose diseases. Pathologists look at tissue from the body that is removed during surgery or a biopsy. Samples of your breast tissue and lymph nodes will be sent to the pathology lab for review. The pathologist writes up a summary of their findings, which is called a pathology report.
You should get a copy of your pathology report for your records and to share with your healthcare team. Understanding this report can help you when making treatment decisions.
What will you find on a pathology report?
The report has a few sections:
- Some information about you, like your health history.
- Diagnosis (suspected or known).
- The procedure that was done to get the tissue sample.
- What the tissue looks like to the naked eye (called gross description).
- What was seen under the microscope (microscopic description).
- A pathologic diagnosis (a diagnosis based on what the pathologist saw under the microscope).
For breast cancer, the report will also have:
- The type of cell the cancer comes from.
- The tumor size and grade.
- Whether cancer cells are in the lymph system or blood vessels.
- Information about surgical resection margins (the edge of the tissue that was removed).
- Hormone receptor and Her2 status.
Breast cancer pathology reports contain a lot of information and can be hard to understand. To help you better understand, let's go through some of the sections you might find in your report.
The Gross Description
The gross description describes what the pathologist received and saw with the naked eye.
- In a biopsy, the sample is often a small piece of tissue. The pathologist may describe the color, shape, feeling, and size of the tissue.
- After breast cancer surgery, large pieces of tissue and lymph nodes may be described in the report. This description might mention "inked" margins or sutures, which the surgeon adds so the pathologist can tell "which end is up" after the tissue is taken out of the body. The report may also mention surgical clips or wires that were used by the surgeon to be sure that the correct area was taken out.
- After a sentinel node biopsy, the gross description may say a lymph node is "hot,” which refers to the radioactive tracer that is used by the surgeon to find the sentinel node. A lymph node may also be called "blue” if a blue dye was used to find the node. The pathologist may describe how they divided the tissue for further analysis.
The gross description tells you the size of the tissue being looked at, but not the size of the actual cancer. The gross description isn't helpful in telling you about the stage of your cancer or which treatment might be best. We will discuss these in the next sections.
Microscopic Diagnosis
This section may be called “microscopic diagnosis,” “description,” or just “diagnosis.” This part of the report has the most useful information for you. Not every report goes through the microscopic diagnosis in the same order. Some use different terms to describe the same thing. In this section, we will go over each part of the microscopic diagnosis section in detail. Sometimes the tests are done in different labs or take different lengths of time to complete, so you may not get all your results at once. It is important to wait for all the results to best understand your cancer.
Type of Breast Cancer
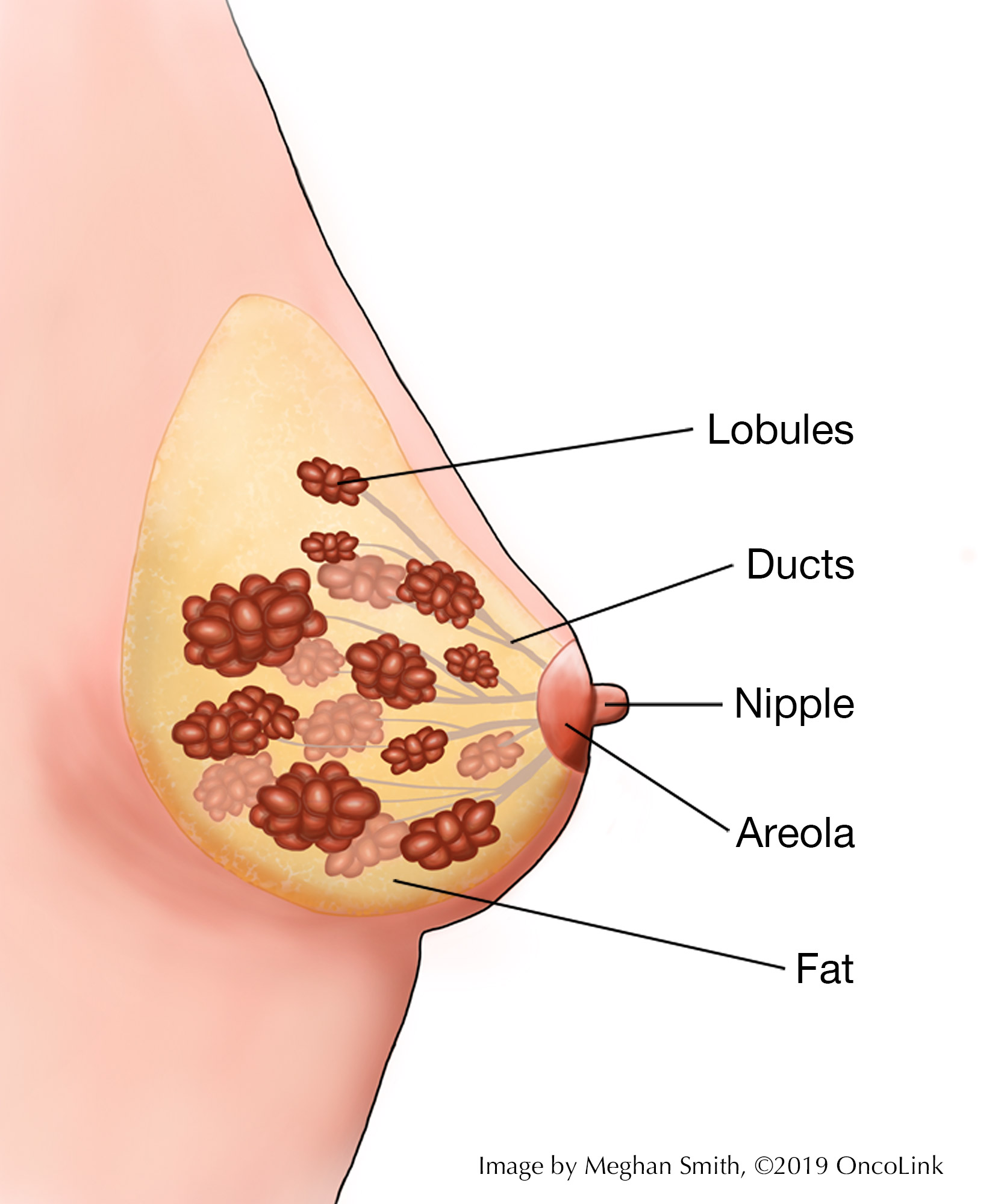
Almost all breast cancers start in glandular tissue, and are called adenocarcinomas (cancer of the glandular tissue). They are further named by where they start in the breast and how they look under the microscope.
- Breast tissue is made up of lobules, which produce milk; and ducts, which carry the milk to the nipple.
- Breast cancer starts in a duct or a lobule and this, along with how it looks under the microscope, determines the type of breast cancer it is. The type can help guide some of your treatment choices.
- Breast cancer can be non-invasive, which means it does not spread beyond the lobule or duct, or invasive, which means it has spread beyond the lobule or duct.
Types of Non-Invasive Breast Cancer
Ductal Carcinoma In Situ (DCIS)
DCIS is the most common type of non-invasive breast cancer. It is sometimes called intraductal carcinoma. It is malignant (cancerous), and as it grows, the center of the tumor starts to die because it outgrows its blood supply. This area of dead tissue, called necrosis, can calcify (harden), which can be seen on a mammogram (x-ray of your breast). DCIS tumors are further identified by how the cells look under the microscope, classifying them into subtypes. These subtypes are: comedo, papillary, micropapillary, solid, and cribiform. Many tumors will be a mix of two or more subtypes. In general, all types of DCIS are treated similarly.
Lobular Carcinoma in Situ (LCIS)
Cancer classified as LCIS doesn’t usually have areas of necrosis or calcifications, so they are not easily seen on mammograms. LCIS is not considered a true cancer, it is an accumulation of abnormal cells in the lobule. It is considered a risk factor for developing breast cancer in the future in either breast. LCIS is often found by chance by a pathologist in a tissue sample that was removed for another reason.
Types of Invasive Breast Cancers
Infiltrating Ductal Carcinoma (IDC)
IDC is the most common type of invasive cancer, making up about 80% of cases. This tumor starts in the duct and spreads beyond the duct into normal breast tissue.
Infiltrating Lobular Carcinoma (ILC)
ILC is less common, making up about 10% of cases. This tumor starts in the lobule and spreads beyond the lobule into normal tissue.
Medullary Carcinoma
Medullary carcinoma is rare, making up only 1-7% of all breast cancers. These cancers often have a well-defined boundary between the cancer cells and the normal cells. This type of cancer will not be given a histological grade by a pathologist (discussed below).
Inflammatory Breast Cancer (IBC)
IBC is also rare, making up 1-5% of breast cancer cases. IBC presents differently than other types of breast cancer. Common symptoms include swelling or enlargement of one breast, reddened, warm to the touch, itchy and tender skin, and is often without a lump. In some cases, the skin becomes thickened and dimpled, appearing like an orange peel. IBC tends to be an aggressive form of breast cancer.
Tubular Carcinoma (TC)
TC is a rare type of invasive breast cancer, making up about 2% of cases. Its name comes from the pathologist seeing a "tubular pattern" in 75% or more of the specimen. TC does not often spread (metastasize) to other areas of the body.
Mucinous Carcinoma (MC)
MC may also be called “colloid carcinoma.” MC is a slow-growing tumor. This tumor is rare and is named for the mucin (protein and sugar compound) produced by and surrounding the tumor cells. These tumors rarely spread (metastasize) to other parts of the body.
Other Rare Subtypes
- Metaplastic - A rare type of IDC.
- Adenoid Cystic – A rare type of tumor that most often occurs in the salivary gland.
- Papillary.
- Secretory.
- Paget's Disease: Development of red, weeping or crusty lesions on the breast tissue or nipple. While not a cancer itself, this is linked to an underlying breast cancer.
Histological Grade
The histological grade is reported using the "Bloom Richardson Scale" or "Nottingham Score.” It is a combination of nuclear grade, mitotic rate, and tubule formation, which describe what the tumor cells look like under a microscope. Histological grade predicts how aggressive the tumor cells are. This scoring system is detailed and often does not affect treatment decisions. However, you will see it on your report and may want to know what it means. In general, high grade tumors are more likely to recur (come back) compared to low grade tumors.
- Nuclear Grade: A score is given from 1 to 3, based on what the nucleus of the cancer cells looks like compared to normal cells. In nuclear grade 1, the nucleus of the cancer cells looks more like normal cells, while in nuclear grade 3, it looks the least like normal cells.
- Mitotic Rate: Describes how quickly the cancer cells are multiplying or dividing using a 1 to 3 scale: 1 being the slowest, 3 the quickest.
- Tubule formation: This score tells you the percent of cancer cells that are formed into tubules.
- A score of 1 means more than 75% of cells are in tubule formation.
- A score of 2 is between 10 and 75%.
- A score of 3 is when less than 10% of cells are in tubule formation.
The three scores (nuclear grade, mitotic rate, and tubule formation) are then combined for a total score between 3 (1+1+1) and 9 (3+3+3). This score makes up the histological grade. You may see the three values and total score, or just the final grade.
- Score of 3,4 or 5: Well differentiated or low grade (Grade 1).
- Score of 6 or 7: Moderately differentiated or intermediate grade (Grade 2).
- Score of 8 or 9: Poorly differentiated or high grade (Grade 3).
Tumor Size
The size of the tumor is listed in centimeters. 2 ½ centimeters is about 1 inch. Sometimes the pathologist finds more tumor(s) in the sample that you did not know were there. If many tumors are found, the size and location of each will be noted. Tumor locations are often based on the quadrant (area) it was found in. Imagine the breast is divided with a "+" sign into 4 parts or quadrants. They are named upper inner quadrant (UIQ), upper outer quadrant (UOQ), lower outer quadrant (LOQ), and lower inner quadrant (LIQ). The breast tissue that is under the armpit is called the "axillary tail.”
Margins
Margins are the edges of the surgical cuts the surgeon made. The report will tell you how close the tumor comes to these edges. During cancer surgery, the surgeon tries to remove the whole tumor and some normal tissue around it. This area of "normal tissue" is important because cancer cells may be in this tissue too. If the edge (or margin) has part of the tumor, there may have been cancer cells left behind. The goal of surgery is to make a "clear margin,” that is, clear of any cancer cells. A "clean" or "clear" margin is when there are no tumor cells within 1-2 millimeters (depending on the pathologist) of the edge of the sample. If the tumor cells are closer than this to the margin, more surgery or radiation may be needed.
Lymphovascular Invasion
When the pathologist looks at the tumor and surrounding tissue in the sample, they look at the tiny blood vessels and lymphatic drainage to see if there are any tumor cells in them. This is different from the lymph nodes and is reported as whether or not lymphatic or vascular invasion is seen. If there are tumor cells in the small blood vessels or in the lymphatic drainage, it may be a sign of a more aggressive tumor.
Lymph Nodes
The lymph system is the "housekeeping system" of the body. It is a network of vessels (tubes) that connect lymph nodes. These nodes can vary in size but are often up to about 2 centimeters wide. They have cells that clear bacteria and other foreign debris from the body. Lymph is a watery liquid that flows between cells in the body, picking up things that shouldn’t be in your body and moving it into the lymph node for filtering. This waste leaves the body through the liver.
Cancer cells use the lymph system to travel to other areas of the body. During breast cancer surgery, lymph nodes are removed and checked for cancer cells. This will be reported as the number of lymph nodes that had cancer cells in them and how many were looked at. For example, the report might state "ten benign lymph nodes (0/10)" (no cancer seen) or "tumor seen in ten of twelve lymph nodes (10/12)."
In some cases, sentinel lymph node biopsy may be used. During this procedure, a dye and/or radioactive tracer is put into the same area as the tumor, allowing it to naturally drain to the lymph nodes. The first 1 or 2 lymph nodes it travels to are called the sentinel node(s). The idea is that the cancer cells would travel the same path, so if cancer cells are not present in the sentinel node, it can be assumed that they did not spread into the lymph system. If the pathologist finds cancer cells in the sentinel node, a full axillary lymph node dissection is recommended.
Hormone Status
There are high numbers of hormone receptors for the hormones estrogen and progesterone in some breast cancers. These tumors need hormones to grow. These tumors are known as hormone receptor-positive, ER+/PR+, ER+/PR- or ER-/PR+. ER stands for “estrogen receptor” and PR stands for “progesterone receptor.” The receptors are on the cancer cells and when the hormone attaches to the receptor, the cancer cell can grow and divide. Hormone therapy can be used to block these receptors, slowing or stopping tumor growth or preventing recurrence (cancer coming back).
There is no standard for reporting the receptor status, so you may see any of these:
- A percentage of the cells that tested positive for receptors (from 0% to 100%).
- A number between 0 and 3, with 0 being no receptors and 3 being the most receptors.
- An “Allred score” is a combination of the percent positive and their intensity. The score is from 0-9, with 9 being the most strongly receptor positive.
- Positive or negative.
In the case of just a positive or negative result, the percentage should be requested. This is because research has shown that even tumors with very low positivity can benefit from hormone therapy, yet some labs report low results (<10%) as negative. Therefore, the only true negative is a result that is zero percent of receptors positive.
Her-2 Status
The Her-2/neu gene increases the production of a protein found on the surface of breast cancer cells that tells the cells to grow and divide. In about 10-20% of breast cancers, there are too many copies of the gene, or the protein is overexpressed on the cell surface. This causes the cancer to grow faster and be more aggressive. Breast tumors are often tested, by one of two tests, to see if they have too many copies of the gene or overexpress the protein:
- The immunohistochemistry (IHC) test looks for overexpression of the protein and is reported as a number from 0 to +3. Zero and +1 are considered Her 2 negative, +2 is borderline and +3 is considered Her 2 positive.
- The second test, called FISH (or fluorescent in situ hybridization), tests the tumor for extra copies of the Her 2 gene and is reported as positive or negative.
Patients with a +2 (borderline) result on IHC, should also have the FISH test done to clarify the borderline result as positive or negative. Her 2 positive tumors may be treated with medications, called monoclonal antibodies, targeting the Her 2 protein.
Stage of the Tumor
The staging system usually used for breast cancers is the American Joint Committee on Cancer (AJCC) staging system. This system uses the extent of the primary tumor (Tis-4), the absence or presence of cancer in the lymph nodes (N0-3), and the existence of metastasis (M0 or 1) to assign a TNM rating, which corresponds to a stage.
Putting it All Together
Some parts of the report are used to figure out the stage of your cancer. Most parts of the report play a role in deciding what treatment is needed. By understanding the basics of the report, you will be better able to talk about your treatment options with your healthcare team.
Read OncoLink's Overview of Breast Cancer.
OncoLink is designed for educational purposes only and is not engaged in rendering medical advice or professional services. The information provided through OncoLink should not be used for diagnosing or treating a health problem or a disease. It is not a substitute for professional care. If you have or suspect you may have a health problem or have questions or concerns about the medication that you have been prescribed, you should consult your health care provider.
Information Provided By: www.oncolink.org | © 2025 Trustees of The University of Pennsylvania