Intracavitary Brachytherapy for Gynecologic Cancers – Tandem and Ovoid or Ring
What is brachytherapy?
Brachytherapy is the use of radiation that is put directly inside your body using applicators. This allows a higher dose of radiation to reach the area where your tumor is or was before surgery. Brachytherapy for gynecological cancers helps reduce radiation from affecting healthy tissues, such as your bowel and bladder.
In the treatment of gynecological cancers, brachytherapy may be given with external beam radiation. How often you receive brachytherapy will be determined by your care team. You may receive it several days in a row. In this case, you would likely stay in the hospital until you have gotten all your treatments. In other cases, you may receive it once a week for many weeks. In this case, you could go home between treatments. Ask your provider what your treatment schedule will be before you start treatment.
What is a tandem and ovoid or ring applicator?
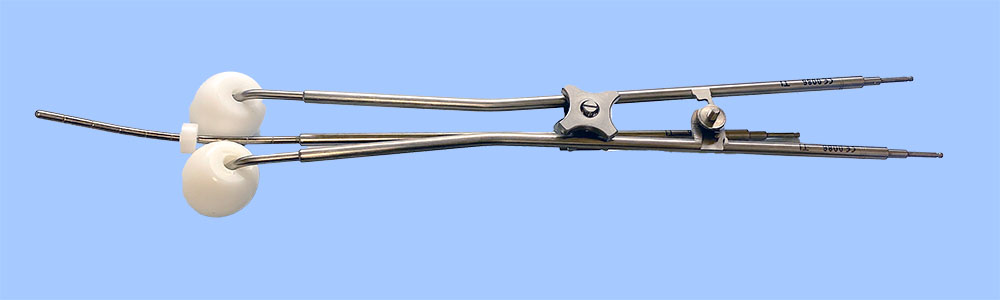
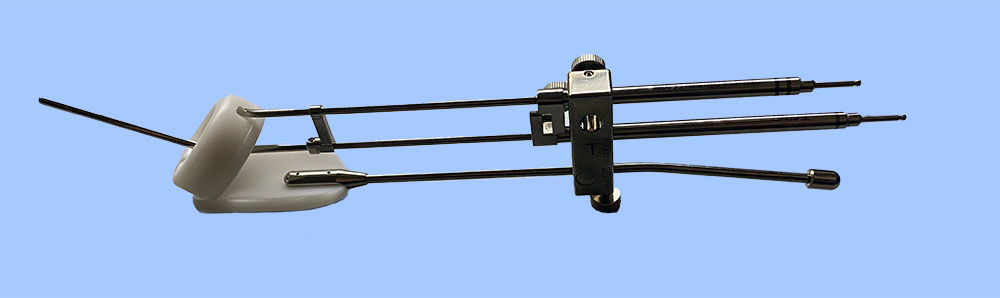
Applicators are used to place the radiation inside your body. For some gynecologic cancers the applicators used are "tandem and ovoid" (T&O) or a "tandem and ring" (T&R). A tandem is a long, thin metal tube that is put through your cervical canal into your uterus. Ovoids are circular hollow capsules, and a ring is a hollow ring. Either the ovoids or the ring will be placed in your vagina, pressing against your cervix.
How is the applicator placed?
Before brachytherapy can start, your applicator is put into place in an operating room. An IV (intravenous line) is placed and you are given sedation (something to make you calm or go to sleep). You may also be given medications to manage pain and nausea. A catheter with a bag at the end of it will be placed in your bladder to collect your urine. If you are receiving treatment for a few days in a row, you may also have a rectal tube placed to collect your stool. You may be given medications to reduce your stool output.
A tandem will be placed in your uterus and the ovoid or ring in your vagina against your cervix. Balloons or gauze may be used to keep them in place. While the applicators are in place you will remain on bed rest to make sure they don’t move. You may be allowed to elevate (lift) the head of your bed, but only a little bit.
In some cases, your provider may use a "Smit sleeve,” also called a stent. It is a plastic hollow tube that is fitted to your uterine cavity and placed while you are under anesthesia. It is often placed at the time of the first applicator placement. The Smit sleeve is fitted into your cervix and sutured (stitched) in place and is not removed until after the last T&O or T&R procedure. A Smit sleeve is used to allow for easier, more comfortable placement of the applicator during treatment. You will likely not feel the Smit sleeve once it is in place. Anesthesia is not needed when removing the Smit sleeve.
Before Treatment
After the applicator is placed and you have woken up from the sedation you will need a series of imaging tests, MRIs and/or CTs, to check that the applicator is in the right place. After the imaging, your care team will make your brachytherapy treatment plan. This can take a few hours. You can have a visitor with you during this time or you can bring some light activities to keep you busy such as a book or tablet.
How is the treatment done?
Once the applicator placement has been confirmed and your treatment plan has been made, you will be taken into a lead-lined room where you will get your brachytherapy treatment. The applicator will be connected to a machine using small cables that feed the radiation source into your applicator. The treatment can last anywhere from a few minutes up to 25 minutes depending on your treatment plan. Once the time is up, the source is removed from the applicator, and it goes back into the machine.
Keep in mind that you will be by yourself in the treatment room as the brachytherapy is being given. This is to protect the staff from the effects of the radiation. Make sure that you have no needs before the treatment starts and that you are comfortable. You will be able to talk with the therapists the entire time and if you have any concerns, you can tell them. The therapists will be watching you during treatment from the cameras in the room.
After Treatment
If you are receiving treatment a few days in a row the applicator will not be removed until after your last treatment. You will stay on bed rest until all your treatments are done. If you are having treatments once a week then the applicator will be removed after each brachytherapy treatment. In either case, the IV, any catheters, and the applicator will be removed by your care team. You are not radioactive after treatment, and it is safe to be around your friends and family.
You may need to stay for a short time after treatment to be monitored for bleeding, to be sure you can urinate on your own after the catheter is removed, and to be sure you can move around safely after any medications you received. You will not be able to drive a vehicle or do any heavy activity, so be sure to have someone with you that can drive you home.
What can I expect after the treatment?
Your provider should talk with you about what you can expect after treatment, this may include:
- Spotting, bleeding, or vaginal discharge after the applicator is removed. This should not be more than a normal menstrual period. Sanitary pads should be used instead of tampons because they can cause more irritation in your vagina.
- Cramping, like menstrual cramps, for 24 hours after the procedure. You may use ibuprofen (Advil, Motrin, or Nuprin) or naproxen (Aleve or Naprosyn) to relieve the cramps. Be sure to follow the instructions on the bottle.
- Diarrhea. You can take over-the-counter medications, such as loperamide (Imodium) or Kaopectate to help manage any diarrhea. See our managing diarrhea teaching sheet for other tips on managing diarrhea.
- No sexual intercourse (or placing anything into your vagina) during treatment and for a time after treatment. It could cause tenderness and irritation in your vagina.
- To be given vaginal dilators to use once your treatment is done. These will help your vaginal tissue stay flexible, making intercourse more pleasant, but also making pelvic exams more comfortable. You will need to use the dilator for the rest of your life. See our teaching sheet on dilators to learn more about them.
- Burning when you urinate for up to 24 hours if you had a foley catheter during the procedure. You should drink 8-10 glasses of nonalcoholic and caffeine-free beverages a day for a few days after the procedure to ease any burning.
After treatment, you can eat a normal diet. Ask your provider when it is safe to have intercourse, go swimming, take a bath, or douche. For some women, douching with vinegar and water will be recommended to help clean out any dead tissue after your brachytherapy treatments are done. Your provider will tell you if this is right for you. You can buy a douche kit at your local pharmacy.
When should I call my care team?
Reasons to call your care team:
- If you develop a fever (temperature > 101°F / 38.3°C).
- You have pain that is not relieved with over-the-counter medication.
- You have a lot of bleeding (more than a menstrual period) or develop a vaginal discharge.
- You have burning or blood in the urine more than 24 hours after the procedure.
- You do not have a bowel movement for 3-4 days after the procedure.
- You have more than 3-4 episodes of liquid diarrhea in a day.
The process and techniques used to deliver brachytherapy using a tandem and ovoid or ring can be specific to the center where you are getting your treatment. Do not hesitate to ask questions regarding your care.
OncoLink is designed for educational purposes only and is not engaged in rendering medical advice or professional services. The information provided through OncoLink should not be used for diagnosing or treating a health problem or a disease. It is not a substitute for professional care. If you have or suspect you may have a health problem or have questions or concerns about the medication that you have been prescribed, you should consult your health care provider.
Information Provided By: www.oncolink.org | © 2025 Trustees of The University of Pennsylvania