Surgical Procedures: Surgical Staging for Ovarian (Epithelial), Primary Peritoneal and Fallopian Tube Cancer
Ovarian (epithelial) cancer, fallopian tube cancer, and primary peritoneal cancer are gynecologic cancers that happen when cancerous cells grow on the surface of the ovary, lining of the fallopian tube, or the peritoneum. These cancers are treated in the same way.
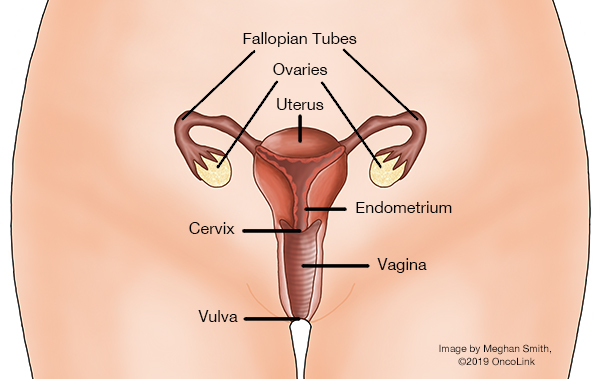
The ovaries and fallopian tubes are part of the female reproductive system. The ovaries are two almond-shaped organs that hold and release eggs for ovulation. They also make hormones. The fallopian tubes are on either side of the uterus. The eggs travel from the ovaries to the uterus through the fallopian tubes. The peritoneum is the tissue lining the abdominal wall, covering the abdominal organs.
What is surgical staging and how is it done?
Staging is a way to find out how far the cancer has spread in your body. Surgery can be used to help stage these cancers. The stages for this cancer are I (1) through IV (4). The number of the stage will be higher in a larger cancer, one that has spread to lymph nodes, and/or moved to other parts of the body (metastasized).
The goals of surgery are to:
- Figure out the stage so a treatment plan can be made.
- Debulk as much of the cancer as possible.
A woman may need more than one type of surgery to treat these cancers. These procedures can include:
- Hysterectomy.
- Total Hysterectomy: Removal of the uterus and the cervix. The ovaries and fallopian tubes may or may not be removed.
- Partial/Subtotal/Supracervical Hysterectomy: Removal of the upper part of the uterus just above the cervix. The ovaries and/or fallopian tubes may or may not be removed.
- Oophorectomy: Removal of the ovaries.
- Unilateral Oophorectomy: Removal of one ovary.
- Bilateral Oophorectomy: Removal of both ovaries.
- Salpingo-oophorectomy: Removal of the ovary and fallopian tube. This can be unilateral (one side) or bilateral (both sides).
- Omentectomy: Removal of the peritoneal tissue that is around the pelvic organs and contains blood vessels, nerves, lymph vessels, and lymph nodes.
- Lymph Node Biopsy: Removal of a lymph node(s) to check for cancerous cells.
- Pelvic and abdominal washings: During surgery, any fluid within the pelvis will be checked. In some cases a "wash" of the abdominal cavity is done with a liquid. This "wash" is sent to the lab to check for cancer cells.
- Other Biopsies: Tissue samples from other parts of the abdomen and pelvis may be removed and sent to the lab for testing.
During surgery, the surgeon will try to take out as much cancer as possible. A debulking surgery can be classified as:
- Optimal: The tumors not removed are no more than 1 centimeter in diameter.
- Sub-optimal: The tumor left is larger than 1 centimeter in diameter.
Women who undergo a debulking may need to have other organs removed. These include either part of or the whole:
- Colon.
- Bladder.
- Spleen.
- Gallbladder.
- Liver.
- Pancreas.
- Stomach.
A hysterectomy can be done in a few ways:
- Abdominal: An incision (cut) in the abdomen is made to remove the uterus.
- Vaginal: An incision (cut) is made in the upper vagina, and the uterus is removed through this opening.
- Laparoscopic: Many small incisions are made in the belly. A laparoscope (thin, lighted tube with surgical tools attached to it) is put in through these cuts.
- Robotic: The surgeon controls a robotic arm to perform the surgery through small incisions.
The type of surgery you have will be based on what type of cancer you have, how far it has spread, and if there is a goal of preserving fertility.
What are the risks/side effects of having surgery for ovarian, primary peritoneal, or fallopian tube cancer?
The main side effect of a hysterectomy is the loss of fertility. The uterus is removed and menstrual periods will stop. If you keep the ovaries, you may not have menopausal symptoms since estrogen is still being made by the ovaries. If the ovaries were removed during surgery, menopause will happen. Your risk of osteoporosis, heart disease, and urinary incontinence is increased once menopause happens.
The risks of surgery include:
- Fever.
- Infection.
- Bleeding.
- Injury to the urinary tract and/or nearby organs.
- Nerve damage.
- Lymphedema (swelling).
- Blood clots.
- Bowel obstruction (blockage).
- Urinary issues.
- Sexual changes such as vaginal dryness and/or loss of interest in sex.
What is recovery like?
You will need to stay in the hospital for three to seven days, depending on the extent of surgery you have had. You may have a catheter in place to drain your bladder of urine. You may need to go home with the catheter.
Early walking and deep breathing can help prevent blood clots and pneumonia.
Your medical team will discuss with you the medications you will be taking (blood clot and infection prevention, etc), pain management, and constipation prevention.
Although your healthcare provider will discuss your activity restrictions, often it is advised that you:
- Get plenty of rest.
- Avoid heavy lifting.
- No tub bathing, sexual intercourse or anything in the vagina (tampons, douching, etc). Bloody to light vaginal discharge is normal.
- Do not drive while taking narcotic pain medication.
Women generally can expect to recover from an abdominal hysterectomy in 4 to 6 weeks, whereas recovery from a vaginal hysterectomy is about 3 to 4 weeks.
What will I need at home?
- Thermometer to check for fever, which can be a sign of infection.
- Loose clothes and underwear.
- Incision care items.
- Sanitary pads for vaginal bleeding/discharge.
Care of Incision
- Keep the incision clean and dry. Follow instructions given to you for showering.
- If you have drains, follow the directions given to you for care and emptying.
- Wear loose fitting clothes that won’t irritate your incision.
- Do not apply lotions or ointments to your incision unless your team tells you to.
- Call your care team for any change in your incision including redness, swelling, drainage or opening.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.
OncoLink is designed for educational purposes only and is not engaged in rendering medical advice or professional services. The information provided through OncoLink should not be used for diagnosing or treating a health problem or a disease. It is not a substitute for professional care. If you have or suspect you may have a health problem or have questions or concerns about the medication that you have been prescribed, you should consult your health care provider.
Information Provided By: www.oncolink.org | © 2025 Trustees of The University of Pennsylvania