All About Mucositis
What is the mucosa?
The mucosa is the thin outer layer that lines most organs including your mouth, throat, esophagus, stomach, and bowel. The mucosa is made up of epithelial cells that make mucous. Epithelial cells divide and grow quickly. If you bite your lip, the tissue is often able to heal by the next day because of this quick growth.
What is mucositis?
Mucositis is when the mucosa is inflamed. It can cause mouth sores, oral mucositis, or esophagitis. It can range from a red, sore mouth and/or gums to open sores that can cause you to be unable to eat. Chemotherapy and radiation therapy kill not only cancer cells, but other healthy cells that divide quickly, including the lining of the gastrointestinal (GI) tract. These cancer treatments can cause mucositis.
Oral mucositis can lead to problems such as:
- Pain.
- Nutritional issues from not eating enough.
- Increased risk of infection due to open sores in the mucosa.
Mucositis can affect your quality of life and can be dose-limiting (meaning the dose of chemotherapy may be lowered if you are having mucositis).
What are the signs and symptoms of mucositis?
The signs and symptoms of mucositis can vary but can include:
- Red, shiny, or swollen mouth and gums.
- Blood in the mouth.
- Sores in the mouth, including on the gums or tongue.
- Soreness or pain in the mouth or throat.
- Having a hard time swallowing or talking.
- Feeling of dryness, mild burning, or pain when eating food.
- Soft, whitish patches or pus in the mouth or on the tongue.
- Increased mucus or thicker saliva in the mouth.
Who gets mucositis?
Certain treatments can cause mucositis:
- Radiation to the head, neck, or chest areas.
- Bone marrow or stem cell transplant.
- Certain chemotherapy medications. Ask your provider if your chemotherapy can cause mucositis.
- Total body irradiation.
Factors that can raise your chance of getting mucositis, or that can make it worse if it does occur, include:
- Poor oral or dental health.
- Smoking or using chewing tobacco.
- Drinking alcohol.
- Dehydration.
- Diseases such as kidney disease, diabetes, or HIV/AIDS.
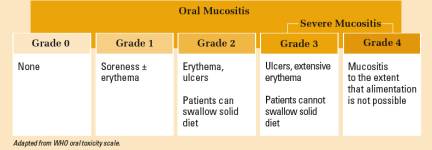
It can be hard to manage mucositis and determine how bad a case is because each person is different. The World Health Organization (WHO) oral toxicity scale is one of many grading systems used to stage the severity of mucositis:
Examples of mucositis:
|
Severe mucositis |
Mucositis with candida infection (thrush) |
Prevention and Treatment
There have been many studies that try different medications and interventions to prevent and help treat oral mucositis. Only a few of these interventions have shown much success.
Oral Care
A good oral care plan can help prevent or decrease how severe mucositis is. It can also help prevent infection through open mouth sores.
Example of oral care protocol:
- Rinse mouth (swish and spit) before and after meals and at bedtime with either:
- Normal saline (1 tsp of table salt to 1 quart (32 oz.) of water).
- Salt and soda (1 tsp of salt and 1 tsp of baking soda in 1 quart of water).
- Use a soft-bristle toothbrush after meals and at bedtime. If the brush causes pain, toothettes may be used.
- Use a non-abrasive (not too rough) toothpaste (or mix 1 tsp baking soda in 2 cups water). Avoid toothpastes with whiteners.
- Keep lips moist with moisturizers such as ChapStick.
- Avoid products that irritate the mouth and gums:
- Avoid commercial mouthwashes and those with alcohol.
- Limit the use of dental floss.
- Do not use lemon or glycerin swabs. Use only a soft bristle toothbrush.
- Increase how much fluid you drink.
- Try to include foods high in protein in your diet.
- Avoid hot, spicy, or acidic foods, alcohol, hard or coarse foods (crusty bread, chips, crackers).
- If you wear dentures:
- Remove whenever possible to expose gums to air.
- Loose-fitting dentures can irritate the mouth and gums and should not be worn.
- Do not wear dentures if mouth sores are severe.
- Do not smoke cigarettes, cigars, or pipes. Do not use smokeless tobacco (chewing tobacco, snuff).
Cryotherapy
Cryotherapy, which is when you suck on ice chips while getting your chemotherapy, has shown some effect in preventing mucositis caused by certain chemotherapies.
Medications
Gelclair® and Zilactin® work by coating the mucosa to form a barrier for exposed nerve endings. In clinical trials, these have helped control pain and increase the ability to eat and speak. Amifostine (Ethyol®), a drug that protects against the damage to the mucosa caused by radiation, is approved by the FDA for patients receiving radiation therapy for cancers of the head and neck. Studies have shown that amifostine can lessen dry mouth and may prevent mouth sores, but more research is needed. Other agents that have been studied include: capsaicin (derived from chili peppers), glutamine, prostaglandin E2, Vitamin E, sucralfate, and allopurinol mouthwash.
Keratinocyte growth factor (KGF) is a substance made in the body that promotes the growth, repair, and survival of cells that protect the lining of the mouth and GI tract. A manmade version of human KGF has been developed as the drug palifermin. It is used for patients with hematologic malignancies or blood cancers (leukemias, lymphomas, and myelomas) who are having bone marrow or stem cell transplants. Palifermin was found to lower the length and severity of mucositis in these patients.
Pain Control
Pain can be a challenge for people with mucositis. In mild cases, ice pops, water ice, or ice chips may help numb the area, but you may need more intervention for relief or pain.
Topical pain relievers (that you put on the mucosa) include lidocaine, benzocaine, dyclonine hydrochloride (HCl), and Ulcerease® (0.6% Phenol). One of the issues of using topical agents is that you can't always coat all areas and the pain relief is brief. If topical agents don’t relieve your pain, your care team may give you oral or intravenous (IV) medications. If you need IV pain medications, you may need to stay in the hospital until the mucosa begins to heal, especially if you are unable to swallow. This side effect is temporary and the use of medications for pain relief is also temporary.
A topical treatment that is often called “magic mouthwash” is a mix of lidocaine, diphenhydramine, and Maalox. This has not been proven to help mucositis or be effective because Maalox can further dry your tissue. It is best to use lidocaine alone or use Mucosal Coating Rinse (MuGard®). To take these medications, use a swish and spit method by swishing it in your mouth for a minute and then spitting it out.
If you are having radiation therapy to the chest/head/neck area or chemotherapy, you should check your mouth at least once a day for redness, sores, or signs of infection. Tell your healthcare team if you have worsening sores, white patches, pus, a "hairy" or thick feeling tongue, bleeding in the mouth, or a fever (temperature greater than 100.4°F [38°C]).
Research continues into many new agents to prevent or treat mucositis, but at this point, it is still a challenging, costly, and distressing side effect.
More Information
Mucositis Tip Sheet: Here you will find helpful tips about oral mucositis (mouth sores). You will find information that explains what oral mucositis is, why it happens, how it is treated, and what you can do to prevent yourself from developing it.
OncoLink is designed for educational purposes only and is not engaged in rendering medical advice or professional services. The information provided through OncoLink should not be used for diagnosing or treating a health problem or a disease. It is not a substitute for professional care. If you have or suspect you may have a health problem or have questions or concerns about the medication that you have been prescribed, you should consult your health care provider.
Information Provided By: www.oncolink.org | © 2025 Trustees of The University of Pennsylvania