Surgical Procedures: Surgery and Staging for Lung Cancer
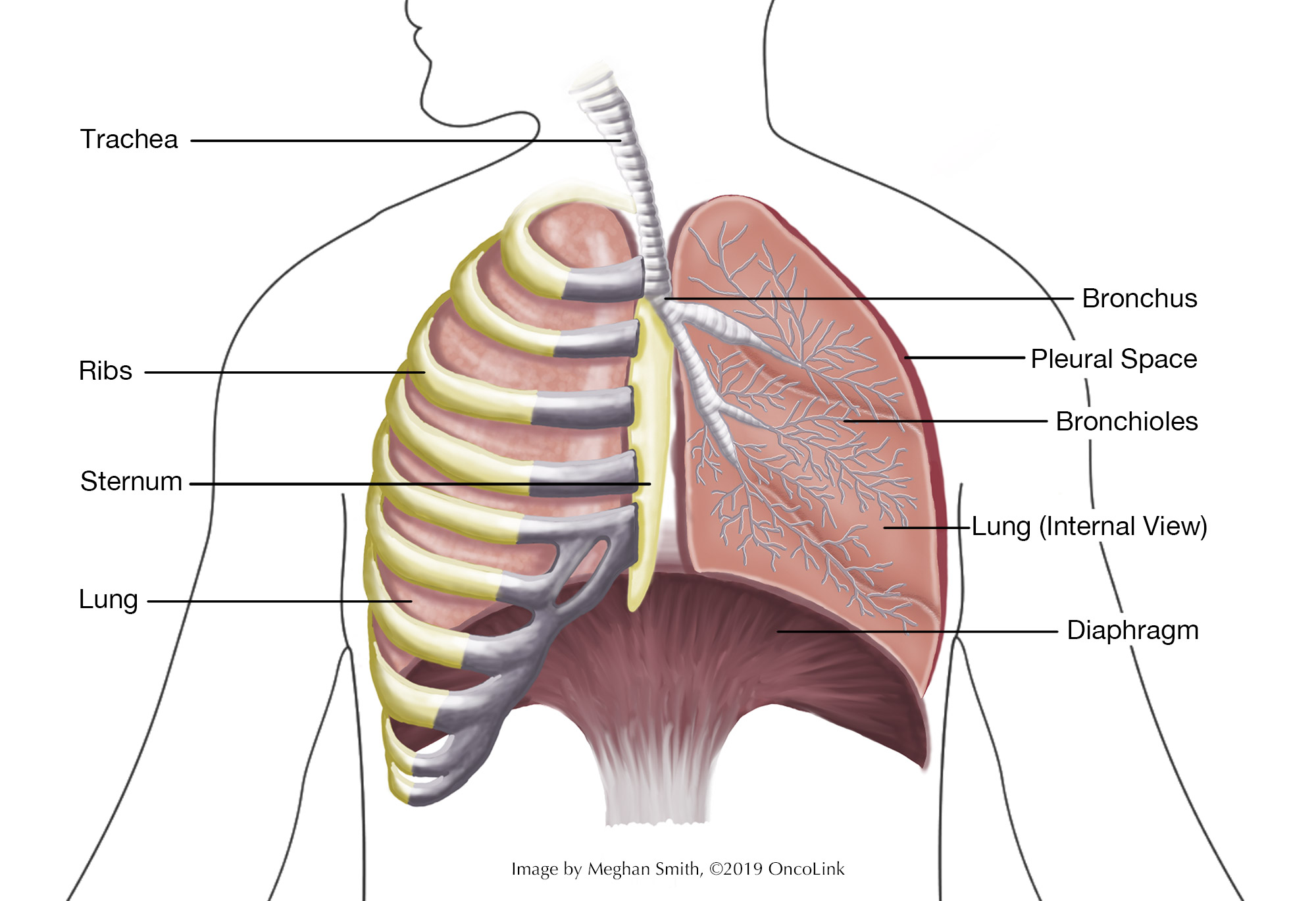
When you have cancer cells in your lung(s), it is called lung cancer. You have two lungs in your chest, one on each side. The lungs take in oxygen and release carbon dioxide.
- Each lung has separate sections called lobes. The left lung has two lobes, and the right lung has three.
- The bronchi are two tubes that attach the trachea (windpipe) to both lungs.
- The internal (inside) parts of the lungs are called the alveoli and bronchioles.
There are two common types of lung cancer:
- Non-small cell cancer (includes squamous cell, adenocarcinoma, and large cell carcinoma).
- Small cell lung cancer (oat cell carcinoma).
Other less common types of lung cancers are:
- Combined small cell/non-small cell carcinoma.
- Lung carcinoid tumor.
- Other non-small cell cancers like pleomorphic cancer, salivary gland carcinoma, unclassified carcinoma, carcinoid tumor, adenosquamous carcinoma, and sarcomatoid carcinoma.
- Adenoid cystic carcinomas.
- Mesothelioma.
- Lymphomas.
- Sarcomas.
To learn more about types of lung cancer visit Oncolink.org.
What is staging and how is it done?
Staging is a way to find out if and how far the cancer has spread in your body. Your provider will have you get a few tests to figure out the stage of your cancer. These tests may include:
Physical Exam: This is a general exam to look at your body and to talk about past health issues.
Imaging: Imaging such as a chest X-Ray and/or CAT scan (CT scan), magnetic resonance imaging (MRI), positron emission tomography (PET), an endoscopic ultrasound, and bone scans may be used to find the extent of your cancer. Intraoperative imaging is a type of imaging done during surgery that may be used to see if there are tumors, if there are none easily seen.
Laboratory Testing: Laboratory testing may be done including sputum cytology, where the sputum is looked at under a microscope for cancerous cells. Other tests used may be light and electron microscopy and immunohistochemistry testing of the tumor.
Pulmonary function testing (PFT): This tests lung function by looking at lung capacity, oxygen use, carbon dioxide waste, and the speed at which air moves through the lungs when inhaling and exhaling.
Procedures: These may include:
- Biopsy: A tissue sample of the lung may be removed during some procedures like bronchoscopy and mediastinoscopy.
- Fine Needle Aspiration (FNA): Tissue or fluid is removed with the guidance of a CT scan, ultrasound, or other radiologic imaging tool. With an FNA, you may have a small incision (surgical cut). Following the procedure, your healthcare team will look for leaking air from the lung with an X-ray.
- Bronchoscopy: A thin, lighted tube is placed down your nose or mouth and into your lung to look at the tumor and take samples of it. This can also be used to take samples of the lymph nodes. There are a few different ways to do a bronchoscopy. Your healthcare provider will tell you which methods are best in your case.
- Thoracoscopy: The surgeon inserts a small camera into the chest wall to look at the area, look at the extent of the tumor, and take biopsies. There are two types of thoracoscopy:
- Video-assisted thoracoscopy or VATS: Can be used for a biopsy or surgery in early-stage lung cancer. This type is like thoracoscopy but fewer/smaller incisions are used, which may result in quicker recovery.
- Robotic-assisted thoracoscopy or RATS: Can be used for a biopsy or surgery. This type is like VATS but the surgeon controls robotic arms that do the surgery.
- Mediastinoscopy: Use of a scope (camera on a tube), placed through the chest wall, to look at the area and take samples of lymph nodes to look for the cancer cells.
- Thoracotomy: This procedure may be needed to check other organs, tissue or lymph nodes and a larger incision is needed to open the chest.
- Thoracentesis: A needle is placed between the lining of the chest and lung, removing fluid to be tested.
- Lymph node biopsy: In some cases, lymph nodes may be removed to test the cancer further.
Lung cancer spreads to other parts of the body through the tissue, lymph, and blood systems. Staging looks at the size of the tumor and where it is, and if it has spread to other organs. It also helps figure out what treatment is best.
Staging for non-small cell lung cancer includes occult/hidden stage through stage IV (4) disease. Small cell lung cancer is described as limited (only on one side of the chest) or extensive stage (found throughout the lung, in the other lung, or in other parts of the body).
Surgical Procedures for Lung Cancer
Surgery is not often used to treat small cell lung cancer.
There are some common surgical procedures used to treat non-small cell lung cancer, such as:
- Wedge Resection: The tumor and a part of healthy tissue is removed.
- Segmental Resection: A more extensive version of a wedge resection, where a larger part of the lung is removed.
- Lobectomy: One lobe of the lung is removed.
- Pneumonectomy: The whole lung is removed.
- Sleeve Resection: Part of the bronchus is removed and reattached to the lung.
What are the risks of lung cancer surgery?
As with any surgery, there are risks and possible side effects. These can be:
- Reaction to anesthesia (Anesthesia is the medication you are given to help you sleep through the surgery, to not remember it and to manage pain. Reactions can include wheezing, rash, swelling and low blood pressure.)
- Pneumonia (lung infection).
- Bleeding.
- Blood clots.
- Infection.
- Shortness of breath.
What is recovery like?
Recovery from lung cancer surgery depends on the procedure you have had. Often, a short hospital stay is needed and full recovery from lung surgery can take several months.
You will be told how to care for your surgical incisions or drains and will be given any other instructions before leaving the hospital.
Your medical team will discuss with you the medications you will be taking, such as those for pain, blood clot, infection, constipation prevention and/or other conditions.
Your team will talk to you about changes to your activity level depending on the surgery you have had. Often:
- Showering should be done with gentle washing of the surgical incision; use only mild soap and warm water. Pat dry with a clean towel.
- Slowly increasing activities, such as walking with periods of rest, is recommended.
- No heavy lifting, yard work or other strenuous activity for 6 to 8 weeks following surgery, or until told otherwise.
- Take all medications as directed.
- If supplemental oxygen is needed, use it as directed.
- Your healthcare team will let you know when it is safe to return to work, driving and sexual activity. Speak with your care team about activity changes you need to make.
Call your healthcare team if you have:
- A fever, incisional redness and/or drainage, which can be a sign of infection. Your care team will tell you at what temperature you should call them.
- Shortness of breath that is sudden and severe.
- Chest pain that is sudden and sharp.
- Chest "fluttering" or an increased (faster) heart rate.
- Any other concerns or questions you may have.
How can I care for myself?
Depending on the extent of your surgery you may need a family member or friend to help with daily tasks until you are feeling better and the medical team gives the go ahead to resume normal activity.
Be sure to take all medications as directed to prevent pain, infection or other conditions and call your medical team with any concerning symptoms.
If constipation is present, speak with your healthcare team about recommendations they have to offer relief.
Deep breathing and relaxation are important to help with pain, keep lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to encourage your child to perform deep breathing and relaxation exercises several times a day in the first week, or whenever you notice you are particularly tense.
- A simple exercise to do on your own: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.
OncoLink is designed for educational purposes only and is not engaged in rendering medical advice or professional services. The information provided through OncoLink should not be used for diagnosing or treating a health problem or a disease. It is not a substitute for professional care. If you have or suspect you may have a health problem or have questions or concerns about the medication that you have been prescribed, you should consult your health care provider.
Information Provided By: www.oncolink.org | © 2025 Trustees of The University of Pennsylvania