Advanced Stage Breast Cancer: Staging and Treatment
What is staging for cancer?
Staging is a way to find out how much cancer is in your body, how far it has spread, and what treatment can be used. Staging looks at the size of the tumor and where it is, and if it has spread to other organs. Tests like biopsies, CTs and MRIs are done to help stage your cancer. Your providers need to know about your cancer and your health so that they can plan the best treatment for you.
The staging system for breast cancer is called the “TNM system,” as described by the American Joint Committee on Cancer. It has three parts:
- T-describes the size/location/extent of the "primary" tumor in the breast.
- N-describes if the cancer has spread to the lymph nodes.
- M-describes if the cancer has spread to other organs (metastasized).
Your healthcare provider will use the results of the tests you have to figure out your TNM result and use these to get a stage from 0 to IV (4).
How is breast cancer staged?
This article will focus on advanced stage breast cancer in women. Learn more about male breast cancer here.
Breast cancer is staged into five groups. Staging is based on:
- The size of your tumor on the mammogram.
- What is found after surgery.
- Any signs of spread to other organs (metastasis).
- Surgery to test if your lymph nodes have cancer cells.
Staging helps guide your treatment choices. Stages 0, I (1), and II (2) are early or moderate stages. Stages III (3) and IV (4) are advanced stages.
The staging system is very complex. Below is a summary of the staging system. Talk to your provider about the stage of your cancer.
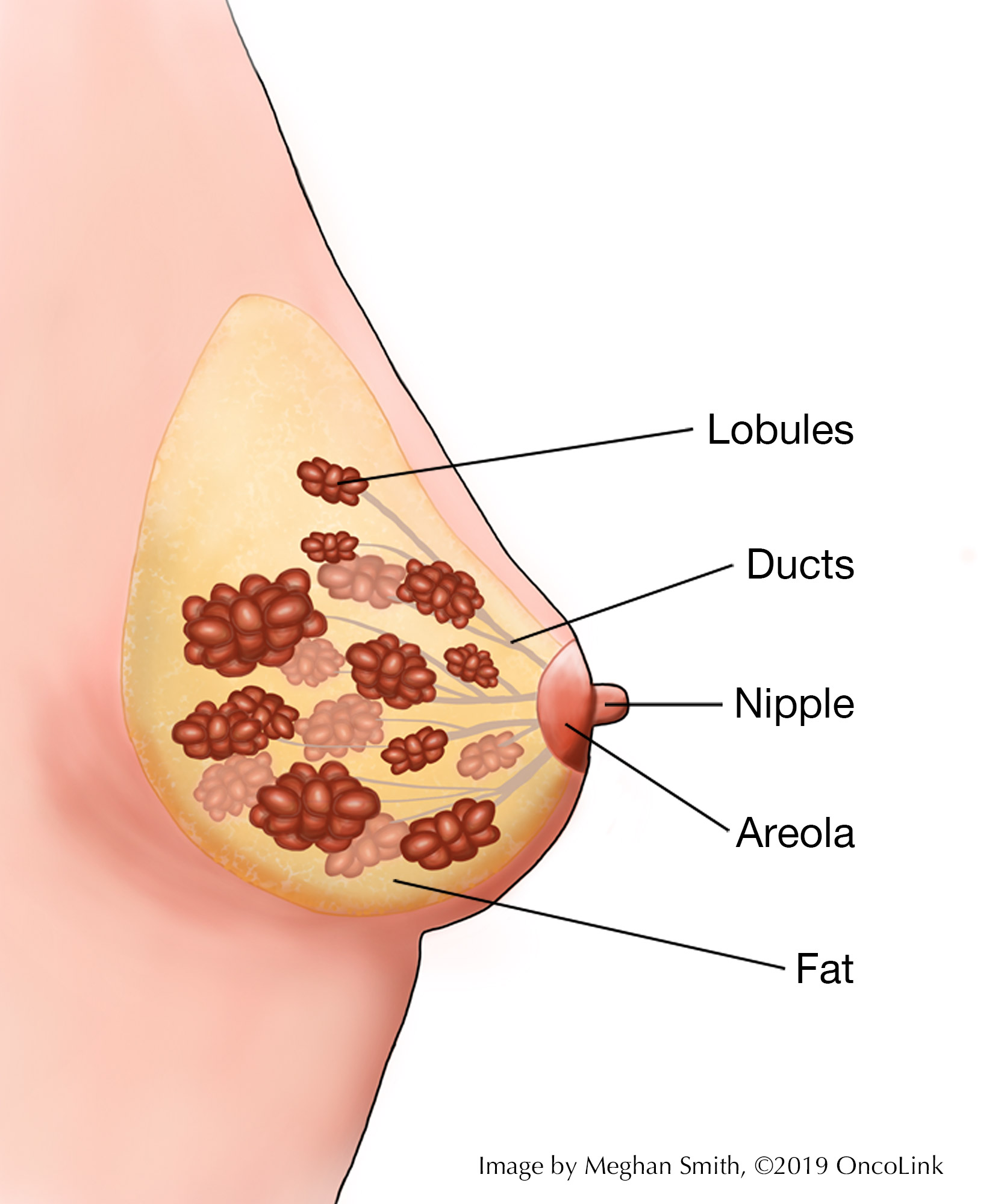
- Stage 0 (called carcinoma in situ/non-invasive breast cancer):
- Lobular carcinoma in situ (LCIS): abnormal cells line a gland in the breast. This is a risk factor for future cancer, but this is not thought to be cancer itself.
- Ductal carcinoma in situ (DCIS): abnormal cells line a duct in the breast. Women with DCIS have a higher risk of getting invasive breast cancer in that breast. Treatment options are similar to patients with Stage I breast cancers.
- Stage I: early-stage breast cancer where the tumor is less than 2 cm and hasn't spread to lymph nodes or other parts of the body.
- Stage II: early-stage breast cancer where the tumor is either less than 2 cm and has spread to 1-3 lymph nodes under the arm; or the tumor is between 2 and 5 cm (with or without spread to the lymph nodes under the arm); or the tumor is greater than 5 cm and hasn't spread outside the breast.
- Stage III: this is called locally advanced breast cancer. The tumor is greater than 5 cm and has spread to the lymph nodes under the arm; or the cancer is found in more than 3 underarm lymph nodes; or cancer has spread to lymph nodes near the breastbone or to other tissues near the breast.
- Stage IV: metastatic breast cancer in which cancer has spread outside the breast to other organs in the body.
Based on the stage of your cancer, your provider may want more tests to see if the cancer has spread to any other organs outside of the breast and nearby lymph nodes. Your providers will talk with you about what is needed to stage your cancer.
This article will focus on treatment for “advanced” stage breast cancer (Stages 3 and 4).
How is advanced stage breast cancer treated?
Treatment for breast cancer depends on many things, like your cancer stage, age, overall health, and testing results. If you have advanced stage breast cancer, your treatment may be different than someone who has early or moderate stage breast cancer. Your treatment may include some or all of the following:
- Surgery.
- Chemotherapy.
- Radiation Therapy.
- Hormone Therapy.
- Targeted Therapy.
- Immunotherapy.
- Clinical Trials.
Surgery
Surgery is used to test lymph nodes for cancer and to remove as much of the cancer as possible. There are many ways that surgery can be done:
- Lymph Node Removal and Testing: If you have invasive breast cancer (any stage except stage 0), you should have lymph nodes removed and tested. This may be done with:
- Sentinel lymph node biopsy: 1-3 lymph nodes are removed.
- Axillary dissection: Many lymph nodes are removed.
- Breast-Conserving Surgery (BCS): You may have the option to have breast-conserving surgery (BCS). If you have BCS, you may need chemotherapy (discussed below) before BCS to shrink the tumor before surgery. This is called neoadjuvant therapy. BCS may be:
- Lumpectomy: The tumor and a part of normal tissue is removed.
- Segmental/partial mastectomy: a larger piece of tissue, but not the whole breast, is removed.
- Modified radical mastectomy: The whole breast is removed, along with some lymph nodes for testing. Many women who have modified radical mastectomies also have breast reconstruction. If you would like reconstruction, you should try to meet with a plastic surgeon before your mastectomy to talk about your options. The reconstruction process can be started at the same time as the mastectomy or done later. Learn more about breast reconstruction.
- Surgery for metastatic disease: In some cases, if you have stage IV disease, you may need surgery to remove tumors that have spread to other areas, (like the brain, spinal cord, and lungs) to help with symptoms or stop the spread of the cancer.
The breast tissue that is removed during surgery and any lymph nodes that are removed will be looked at by a pathologist under a microscope. A report will be written that has:
- The type of cancer cells that are seen.
- The size of the cancer.
- The number of lymph nodes that have cancer in them.
- Information about the cancer such as “grade” (how aggressive the cells look), if it has receptors for estrogen, progesterone (ER, PR), and HER2.
These findings will help decide what treatment will work best for you.
Chemotherapy
Advanced breast cancer means that cancer cells have spread away from where the first tumor started. Cancer can spread (metastasize) to lymph nodes, tissue near the tumor, or other areas of the body. Because of this spread, part of the treatment for advanced breast cancer must be "systemic,” meaning it can travel throughout the body, like chemotherapy.
Your treatment plan may include one or more chemotherapies, called a regimen. A regimen will be given a few times over a certain period (called a cycle). For example, you get a dose of the medicine on day 1 and then have 21 days until the next dose. That 3-week period is called a cycle. You will be watched closely during your treatment for side effects or changes to your blood counts.
- Some patients with advanced breast cancers get a planned number of cycles of chemotherapy. At the end of these cycles, the treatment is stopped. When the chemotherapies are done, you may have surgery (breast-conserving surgery or modified radical mastectomy).
- Other patients will need chemotherapy for the rest of their lives. For these patients, breast cancer may become a chronic illness that never goes away. It can often be controlled for many years with medications that do not cause many side effects. For these patients, one goal of treatment is to manage the cancer and keep a good quality of life.
Many chemotherapy medicines used for breast cancer are given through a vein (intravenously/IV). Some can be given by mouth, in pill form. Some of the common chemotherapies used are adriamycin (doxorubicin), cyclophosphamide, methotrexate, taxanes (taxol and taxotere), capecitabine, fluorouracil, vinorelbine, eribulin, carboplatin, epirubicin, and ixabepilone.
Based on your health, personal values and wishes, and side effects you wish to avoid, you can work with your providers to come up with the best treatment plan for your lifestyle.
Radiation Therapy
Radiation therapy uses high energy x-rays to kill cancer cells. You may need radiation therapy to the breast or the chest wall after a modified radical mastectomy. You may also need radiation to the axilla (armpit) or supraclavicular (lower neck) areas. This radiation can be given at the same time as radiation to the breast or chest wall and is given with the goal of killing any cancer cells that may be in your lymph nodes. In general:
- You will need to go to a radiation therapy treatment center 5 days a week for up to 6 weeks for treatment.
- The treatment is painless and takes just a few minutes.
Your radiation oncologist can answer questions about the benefits, process, and side effects of radiation therapy.
Hormone Therapy
If your tumor has estrogen (ER) and/or progesterone (PR) receptors, it may be treated with hormone therapy. Hormone therapies include tamoxifen and medications called aromatase inhibitors (anastrozole, letrozole, exemestane). These medications are taken in pill form for 5-10 years after breast cancer surgery. They have been shown to lower your risk of recurrence (the cancer coming back) if your tumor has estrogen receptors.
These medications can have side effects. When taking tamoxifen, you may have:
- Weight gain.
- Hot flashes.
- Vaginal dryness and discharge.
Taking tamoxifen may raise your risk of serious medical issues, such as blood clots, stroke, and uterine cancer.
When taking aromatase inhibitors (AIs), you may have:
- Bone or joint pain.
- Thinning of the bones (osteopenia or osteoporosis).
Patients taking AIs should have bone density testing before starting treatment and as needed.
Targeted Therapies
Targeted therapies are medications that target something specific to the cancer cells, stopping them from growing and dividing.
HER-2 is a receptor that is found in about 25% of breast cancers. These are called HER2 positive breast cancers. These tumors may grow faster and are more likely to spread. There are medications that target the HER2 protein. The most common is trastuzumab (Herceptin®), which may be given to treat the cancer or stop it from coming back (recurring).
Other targeted therapies are:
- Everolimus: Targets mTor.
- Abemaciclib (Verzenio®) and ribociclib (Kisqali®): CD4/CD6 kinase inhibitors.
- Olaparib (Lynparza®): PARP inhibitor.
- Palbociclib (Ibrance®) and ribociclib (Kisqali®): CD4/CD6 kinase inhibitors.
- Alpelisib (Piqray®): PI3K inhibitor
Talk with your healthcare provider about targeted therapies and if they may work on your tumor.
Immunotherapy
Immunotherapy uses your body’s own immune system to find and kill cancer cells. It can be given into a vein, taken by mouth, injected under the skin (subcutaneous), or put into a body cavity to treat a specific site. Some of the Immunotherapies used for breast cancer are:
- Dostarlimab-gxly (Jemperli®)
- Pembrolizumab (Keytruda®)
- Atezolizumab (Tecentriq®)
- Fam-trastuzumab deruxtecan-nxki (Enhertu®)
- Margetuximab-cmkb (Margenza™)
- Pertuzumab, Trastuzumab, and Hyaluronidase-zzxf (Phesgo™)
- Pertuzumab (Perjeta®)
- Sacituzumab govitecan-hziy (Trodelvy™)
Talk with your healthcare provider about immunotherapy and if it may be a part of your treatment plan.
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Service.
Making Treatment Decisions
Your care team will make sure you are part of choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It feels like an emergency, but you can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot make the decision for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
You can learn more about breast cancer at OncoLink.org.
OncoLink is designed for educational purposes only and is not engaged in rendering medical advice or professional services. The information provided through OncoLink should not be used for diagnosing or treating a health problem or a disease. It is not a substitute for professional care. If you have or suspect you may have a health problem or have questions or concerns about the medication that you have been prescribed, you should consult your health care provider.
Information Provided By: www.oncolink.org | © 2025 Trustees of The University of Pennsylvania