Implanted Venous Access Device (Port)
Table of Contents
What is an implanted venous access device (port)?
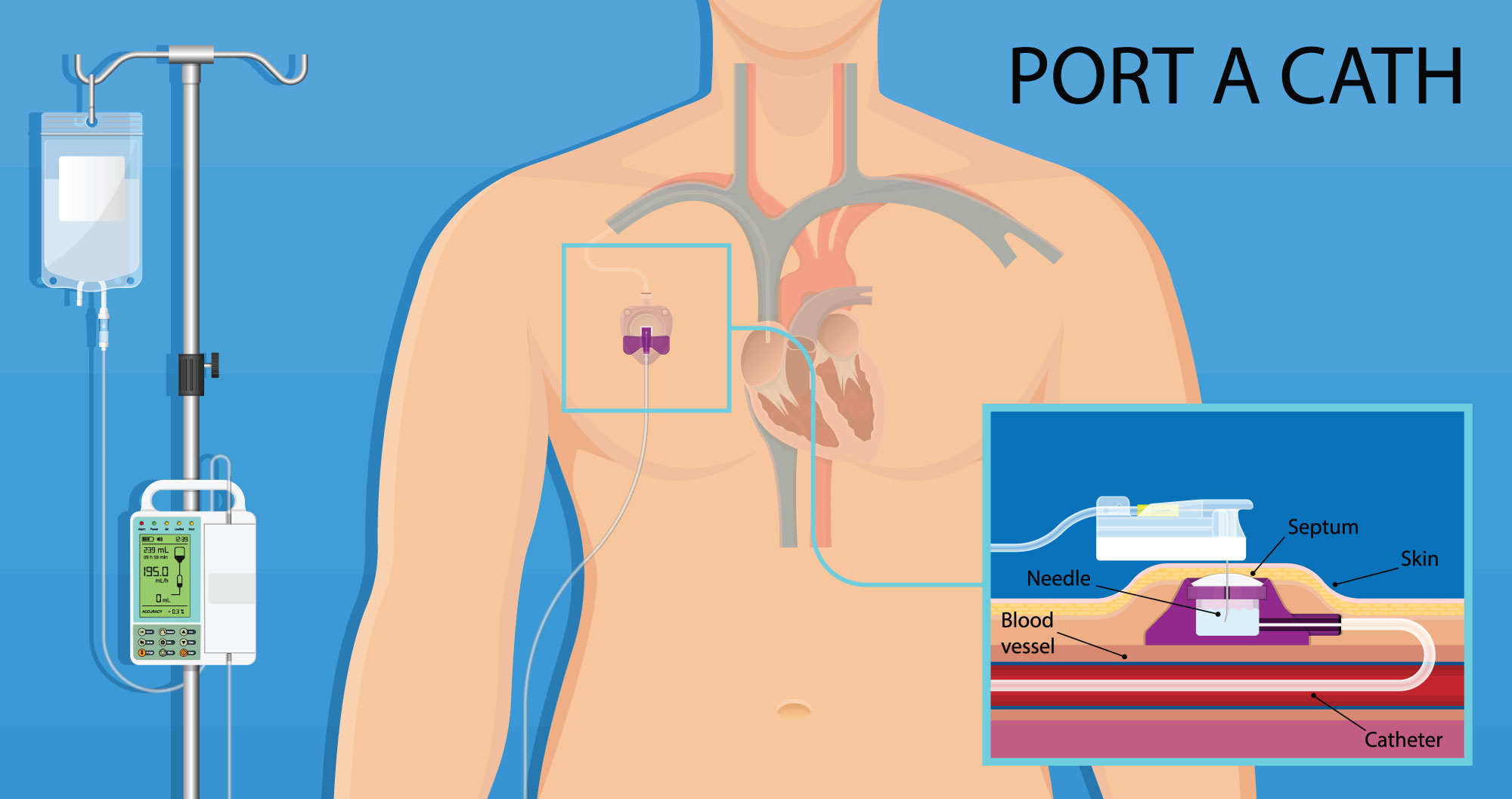
A port, sometimes called a Port-a-Cath, is an implanted venous access device. This means it is placed into your body during a procedure and it gives direct access to a vein. A port is a central line that is used to give medicine and fluid into your veins. It works like an IV catheter but can stay in place for 5 years or more.
A port is made up of a reservoir (object that holds fluid) attached to a tube (catheter). The reservoir is placed under your skin and the tube goes into a vein. The reservoir will look like a bump under your skin. It is round and about the size of a quarter. You usually cannot see the tube. A port makes it easier to get IV medications or to have blood taken. If you are having chemotherapy over a few months or more, your care team may suggest you get a port.
How is a port used?
Often, your port can be used right away. To use your port, a nurse will first "access" the port. This is done by putting a needle through your skin and into the reservoir. Putting the needle in is a sterile (very clean) procedure.
- A numbing medication may be used before putting the needle in.
- The nurse putting in the needle will feel for the reservoir.
- The nurse will put on sterile gloves and clean the area.
- When the area is dry, the needle is put through your skin and into the reservoir.
- The needle is left in place and the area is covered with a dressing.
- The needle is connected to a lumen (clear tube) with a cap at the end. This will be used to give medications, fluids, chemotherapy, blood products, or to draw blood.
- Once your infusion is done or your labs have been drawn, your nurse will remove the dressing and the needle. A Band-Aid may be used to cover the site where the needle was removed.
How do I care for my port?
- Follow your provider’s directions for how you should care for your port after the surgery. This may include avoiding heavy lifting for a while. You should call your provider if you have any signs of infection such as fever, redness, swelling, pain, discharge (drainage), or warmth.
- Wash your hands before handling any tubing attached to the port. When you are finished handling the tube, remove your gloves and wash your hands again.
- While a needle is in your port, be careful to not pull on the tubing to keep the needle from coming out. If the dressing becomes dirty or wet, it should be changed right away.
- A port should be flushed before and after use. Flushing means using a syringe to put saline solution (medical saltwater) into the port.
- Look at your port site each day. Even after the area has healed from surgery, you should check for signs of infection such as redness, swelling, pain, discharge (drainage), and warmth. Also, check that the reservoir is secure under your skin and not moving (a little wiggle back and forth is okay).
- If your port is not being used, it should be flushed with saline once a month. If you no longer need your port, it can be removed.
When should I contact my care team?
You should call your provider if you have any signs of infection. Your provider will tell you at what temperature you should call them. If a flush or fluid given into the port does not flow freely or if the skin around the port is swelling, stop the infusion and call your care team. Contact your care team if you see changes in the area around the port or if the reservoir is moving around underneath your skin.