Transjugular Intrahepatic Portosystemic Shunt (TIPS)
Table of Contents
What is a transjugular intrahepatic portosystemic shunt (TIPS)?
Liver disease can cause high pressure in the veins of the liver. This higher pressure causes a "backup" of pressure before the liver. The blood flowing from your stomach, intestines, and spleen needs to work harder to get through the liver. The veins in the stomach and esophagus (tube that passes food from the mouth to the stomach) become distended (stretched) or enlarged. This stretching or enlargement is called “varices.” Varices can burst and cause life-threatening bleeding. TIPS is a way to control the bleeding caused by liver disease. TIPS stands for:
- Transjugular: Means “through the jugular.” The jugular veins are in the neck.
- Intrahepatic: Intra means “inside” and hepatic means “liver.” Intrahepatic means “inside the liver.”
- Portosystemic Shunt:
- Porto means “portal vein.” The portal vein carries blood from the gastrointestinal (GI) tract, gallbladder, pancreas, and spleen to the liver.
- Systemic means the body’s circulatory system, or the system that carries blood and oxygen throughout your whole body.
- A shunt is a channel or passage for things to pass through.
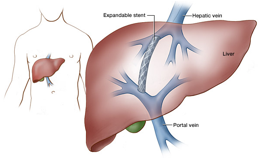
Transjugular intrahepatic portosystemic shunt (TIPS) makes a channel that connects the portal vein and the vein that goes from your liver to the right part of your heart.
A TIPS makes a channel, like a "bypass" between the high- and low-pressure veins in the liver. This bypass is kept open with a stent. A stent is a small, metal tube with a spring-like piece that is covered in a fabric. High-pressure blood entering the liver can now flow through the TIPS. This helps lower the pressure throughout the distended and bleeding veins.
How does my provider know if I need a TIPS?
A TIPS is most often needed when the bleeding veins (varices) can no longer be controlled by medications or endoscopy treatments.
How should I prepare for TIPS?
You may be asked to have lab work, an EKG, and a chest X-ray done before having a TIPS procedure. Ask your provider if it is safe to take your medications before the procedure. You will be told not to eat or drink anything before the procedure, usually starting at midnight the night before.
What happens during the TIPS procedure?
The TIPS procedure is done in the interventional radiology (IR) department by the interventional radiology care team. You will get local anesthesia (numbing medication) in the area where the catheter is placed in your neck. You will also get a sedative (relaxing) medication. Sometimes, general anesthesia is used to put you fully asleep. During the procedure:
- The provider places a small, hollow tube (a catheter, like an IV) through your skin into your jugular vein in your neck. On the end of the catheter is a tiny balloon and a metal mesh tube (stent).
- While taking X-rays, your provider guides the catheter into a vein in your liver.
- A contrast solution (dye) is then injected into the vein so that it can be seen more clearly.
- The balloon is inflated (blown up) to place the stent. This can cause some discomfort.
- The provider uses the stent to connect your portal vein to one of the veins in your liver (hepatic vein).
- Once done, the provider will measure the pressure in your portal vein to make sure it has gone down. A decrease in pressure in your portal vein means the procedure worked as it should.
- The balloon on the catheter is deflated (air is let out) and the catheter is removed through the same vein it was placed.
- After the procedure, a small bandage is placed over the neck area. There are usually no stitches.
Talk with your provider about any questions you have and what you might expect before, during, and after your TIPS procedure.
What are the possible side effects?
The TIPS procedure is complex, but in most cases it can be done with few side effects. Your care team will talk to you about how your procedure went and if you may have any side effects.
This procedure can cause some confusion and lethargy (sleepiness). This is caused by encephalopathy (a change in how your brain works). This can happen because some liver blood is diverted (goes a different way than normal) through the TIPS to lower the pressure in the veins. Toxins that are normally cleared by the liver go around the liver's "filters" and build up in your bloodstream. This can often be treated with a medication that helps clear the toxins. In rare cases, the shunt may need to be reversed.
Other possible side effects include bruising, bleeding, infection, allergic reaction, and kidney damage due to the contrast dye used. Very rare side effects include bleeding in the abdomen (belly), infection of the stent, injury to the main liver artery, and blockage of the stent. Your care team will talk to you about the possible side effects, risks and benefits, symptoms, and when to call them.
Will I need to stay in the hospital?
Often, patients who are having TIPS placement will stay in the hospital overnight and will be discharged the day after the procedure. If you have an emergency surgery, your hospital stay may be longer.
Will I need to have any follow-up visits?
A TIPS can prevent repeat bleeding as long as it stays open. TIPS can cause the blood vessel to become narrow, which can cause bleeding. The narrowing may happen without symptoms. For this reason, you will need regular outpatient follow-up visits with your care team about every 3 to 9 months to make sure the TIPS is working. The follow-up visits become less frequent after the first year or two. Any narrowing within the TIPS is easily treated with an outpatient procedure.