Nipple Preservation and Reconstruction Options
Table of Contents
There are several options for preserving or reconstructing the nipple as part of mastectomy and breast reconstruction. There are also alternatives such as nipple prosthetics and tattooing. The decision about nipple preservation, reconstruction, use of prosthetics, or tattooing is a personal one but is also impacted by the size of the breast tumor, the size of the breast, and other factors. It is important to talk with your healthcare provider about your personal goals and to explore what your options are.
What is a nipple-sparing mastectomy (NSM)?
NSM is a type of mastectomy that preserves the natural skin of the nipple and areola (pigmented skin around the nipple) area of the breast while removing the rest of the breast tissue. This procedure may also be called “total skin-sparing mastectomy.” During this procedure, the breast tissue is removed and the skin, areola, and nipple are left intact.
Who can have an NSM?
- NSM can be used in patients with smaller tumors that are >2 cm away from the nipple and areola area of the breast. You will have an MRI of your breasts to locate the tumor.
- Those who are having a prophylactic mastectomy (due to genetic conditions/BRCA status) and do not have breast cancer.
- Individuals with smaller breasts.
Who is not a candidate for NSM?
- Individuals with tumors that are invading or near the nipple/areola area.
- Individuals with a history of smoking may not be eligible. If you are a former smoker, the amount (pack-years) you have smoked, and how long it has been since you quit are factors in deciding if you are a candidate for NSM. Research has shown that smoking is a major risk factor for complications such as flap skin loss or nipple/areola necrosis after NSM. If you are a smoker and desire an NSM, it is recommended you stop smoking 4-6 weeks prior to the procedure and you cannot begin smoking again after.
- Those who had bleeding or discharge from their nipples with their breast cancer diagnosis.
- Those with large/sagging breasts may be a candidate for NSM, but they also may be at a higher risk for post-surgical complications.
What are the benefits of NSM?
- You may be happier with the look of the breast with your natural nipple.
- Individuals who have NSM report that it has helped them feel better psychologically and lowers distress due to body image.
What are the risks of NSM?
- Infection/ Nipple-areola necrosis: After NSM, there is a risk of infection in the preserved tissue. Necrosis is when the preserved nipple tissue loses blood flow and dies. If this happens, you may need more surgery to treat the infection or necrosis. In some cases, this can lead to the preserved nipple/areola needing to be removed. It is important to talk with your surgeon about your specific risk factors and recovery.
- Risk of residual/recurrent disease: There is always a risk of residual cancer cells remaining after any breast cancer procedure. MRI images may be used before and during surgery to check that as much of the cancer as possible has been removed to help reduce this risk.
- Positioning and appearance: In some cases, you may not be happy with how the nipple is placed or how it looks after reconstruction. The nipple will always be erect after NSM.
- Loss of sensation: While the nipple/areola remains, the nerves that control feeling and sensation in this area are removed with the rest of the breast tissue. This means that you cannot feel the nipple area, or it being touched. This could affect sexual function and well-being.
What are the alternatives to NSM?
- Free nipple grafting: This may be a better option for women with larger or sagging breasts. The nipples are removed (harvested) during mastectomy, checked for cancer cells, and reshaped to leave a thin layer to implant onto a reconstructed breast.
- Nipple reconstruction from skin grafts in flap reconstruction procedures: Skin from other areas of the body, including the labia or the opposite nipple, may be used to reconstruct the nipple.
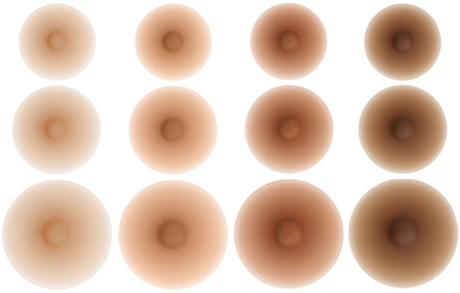
- Nipple prosthetics (artificial nipple): Available in a wide variety of sizes and skin tones. There are many options for nipple prosthetics including custom nipples and nipples you can swim in. They are typically made of silicone and attached to the reconstructed breast or silicone breast with a light adhesive. How long these adhesives last and if they are water safe can vary.
- Nipple tattooing: Uses specialized techniques to tattoo a nipple onto the reconstructed breast.
There are many options for nipple preservation, reconstruction, and prosthetics available to individuals with breast cancer or those considering prophylactic mastectomy. The key is communicating with your provider from the beginning about your goals, concerns about body image, and risks for any of the procedures. Accessing peer support through groups like Living Beyond Breast Cancer (LBBC), After Breast Cancer Diagnosis (ABCD), the American Cancer Society’s Reach to Recovery program, Young Survivors Coalition, and Sharsheret can connect you with other people who have gone through breast cancer and these treatment decisions.