Surgical Procedures: Colectomy
Table of Contents
What is a colectomy?
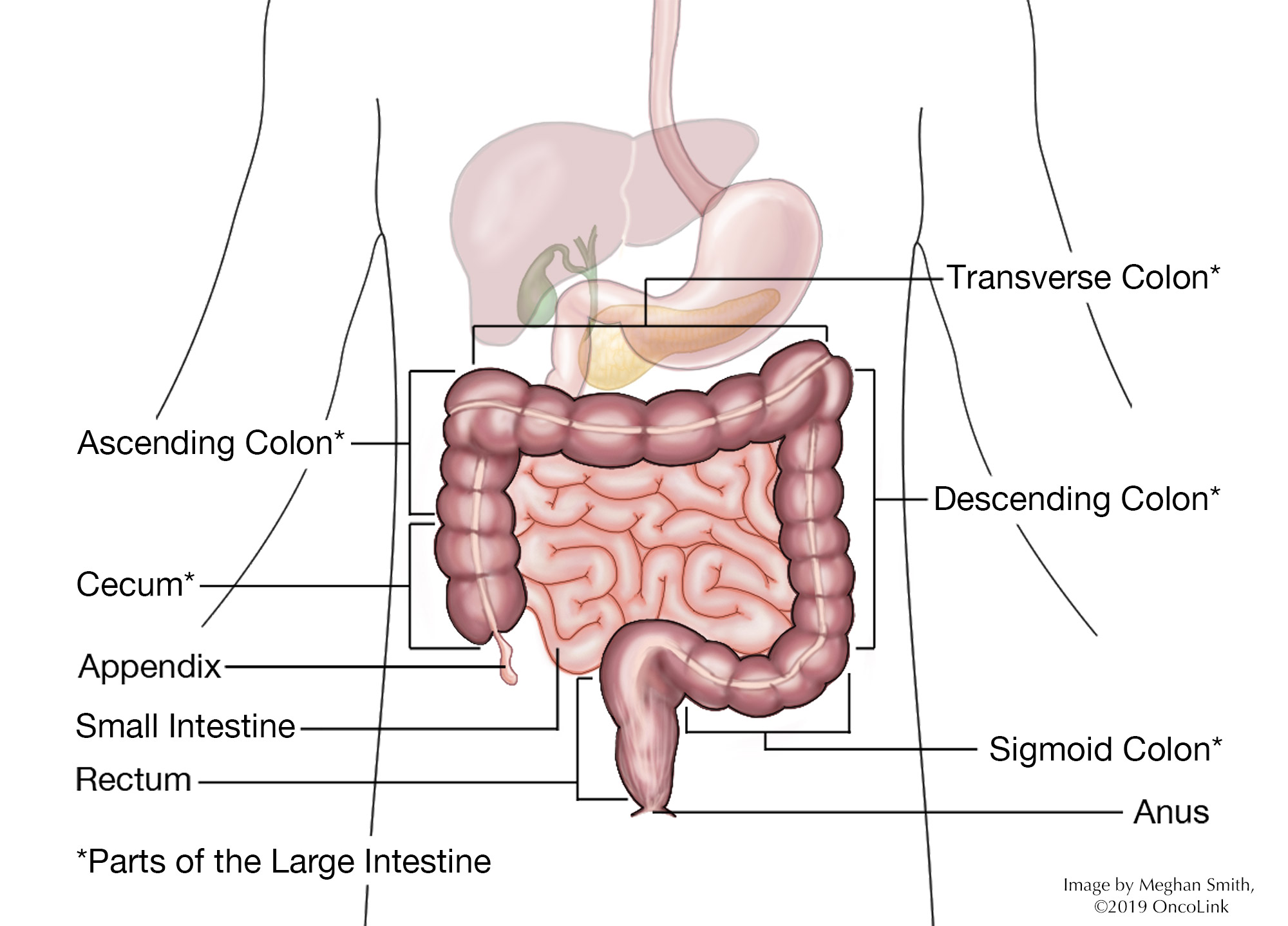
A colectomy is surgery to remove all or part of your colon. The colon is part of your large intestine. Your stool (bowel movement) leaves your small intestine and goes into your colon, where it becomes more solid and gets ready to leave your body through the anus. A colectomy can also be called a large bowel resection.
A colostomy or ileostomy may be needed after colectomy. Both of these procedures create a stoma (opening) allowing stool to pass through, often to a collection device outside of your body. In some cases, the cut parts of the colon will be reattached so that bowel movements can happen, and a colostomy is not needed.
How is it done?
A colectomy can be done using a laparoscopic or open technique.
- Laparoscopic colectomy: A probe with a lighted camera and other surgical tools are put into the abdomen (belly) through many small incisions (cuts).
- Open colectomy: A large abdominal incision is made to do the surgery.
A colectomy may be used to treat:
- Cancers of the colon.
- Precancerous polyps.
- Cases of an inherited (passed down from your parents) genetic mutation where colectomy may stop colon cancer from growing.
- Bowel obstruction (a blockage).
- Infection or bleeding.
- Diverticulitis.
- Crohn’s disease.
- Volvulus (twisted intestines).
- Ulcerative colitis.
- Intussusception (when the intestine folds into itself).
There are many types of colectomy:
- Total colectomy: The whole colon is removed.
- Partial colectomy: Part of the colon is removed.
- Hemicolectomy: The right or left side of the colon is removed.
- Total proctocolectomy: The colon and the rectum are removed. The rectum is the part of the colon that attaches to the anus. The small intestine may be attached to the anus to let stool leave your body normally. A temporary (short term) ileostomy may be needed.
- Abdominal perineal resection: The sigmoid colon (part of the colon that attaches to the rectum), rectum, and anus are removed. A permanent (life long) colostomy is needed after this surgery.
- Segmental resection: A small part of the affected colon is removed.
- Low anterior resection: The uppermost (highest) part of the rectum is removed.
- Sigmoidectomy: The lowest part of the colon is removed.
What are the risks of having a colectomy?
As with any surgery, there are risks and possible side effects. These can be:
- Reaction to anesthesia (Anesthesia is the medication you are given to help you sleep through the surgery, to not remember it, and to help with pain. Reactions can include wheezing, rash, swelling and low blood pressure).
- Bleeding.
- Blood clots.
- Infection.
- Damage to nearby organs like your bladder, ureter, blood vessels, and/or small intestines.
- Incisional hernia (This is when tissue in your belly pushes through the muscle. It can look like a lump and can be painful or tender when touched).
- Adhesion/scar tissue (An adhesion is scar tissue that joins 2 pieces of tissue that should not be joined. They are often painless and do not need treatment. Serious cases can cause a blockage in the bowel or limit blood flow.)
- Your incision opening or coming apart.
- Issues with your colostomy, such as infection and leaking.
- Bowel obstruction (A blockage in the bowel).
- Anastomotic leaks (A leak in the area reconnecting the bowel. This fluid leaks into the body).
What is recovery like?
Recovery from a colectomy depends on the procedure you had. How long you need to stay in the hospital depends on the surgery and the time needed for recovery.
You will be told how to care for your surgical incisions and stoma (if you have one) and will be given any other instructions before leaving the hospital. Full instructions on caring for the stoma (if needed) will be given to you by a specially trained stoma nurse/therapist.
Your care team will talk with you about the medications you will be taking, such as those for pain, blood clot, infection, and constipation prevention and/or other conditions.
Your provider will tell you what you should and should not do when you go home. Often, you should:
- Not lift anything over a certain weight, do any climbing, or any strenuous activity until you are told that you can.
- Change your diet as told. You may be asked to eat a low-residue (low fiber) diet after surgery.
- Drink 8 to 10 glasses of water per day unless told otherwise.
- Not strain to have a bowel movement.
- Not drive while taking pain medication.
- Often, you can return to work in 2-3 weeks, depending on your job.
- Speak with your healthcare team about showering, putting your surgical incisions under water, diet, sexual activity, and stoma care.
What will I need at home?
- Thermometer to check for fever (101°F, 38.3 °C) which can be a sign of infection.
- Loose clothes and underwear.
- Incision and stoma care supplies. These are supplied by the hospital, your healthcare team or the stoma nurse/therapist.
When should I call my provider?
You should call your provider if you have:
- A fever and/or chills. Your care team will tell them at what temperature you should call the office.
- Signs of infection, like redness, bleeding, odor or drainage at the incision.
- Nausea.
- Any new or worsening pain.
- Belly pain and/or swelling.
- Not had a bowel movement for 2-3 days after surgery.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as you are told to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.