Surgical Procedures: Colostomy
Table of Contents
What is a colostomy?
The colon is part of your large intestine. Your stool (bowel movement) leaves your small intestine and goes into your colon, where it becomes more solid and gets ready to leave your body through your anus.
A colostomy is a surgery done to connect the colon to the surface of the abdomen (belly) to let stool pass into a collection bag outside of the body. This is done because the rectum, anus, or the sphincter that controls the passage of stool has been removed or can't be used.
How is it done?
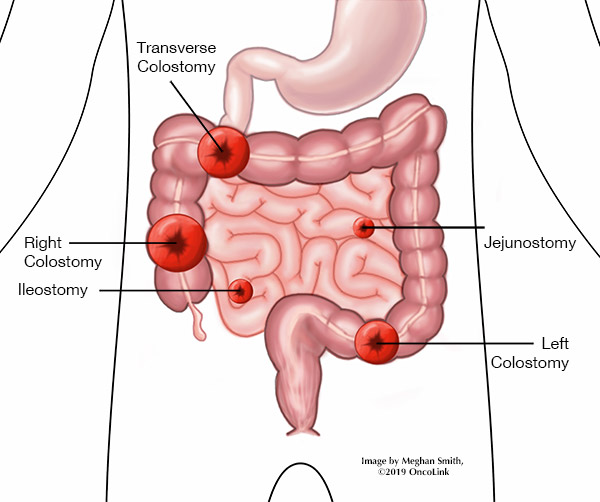
A stoma (hole) is made in your belly wall for stool to pass from the colon to the collection bag on the outside of your body. The stoma can be seen on the outside of your belly. It is made from your intestine. The stoma should be pink to red in color, warm, and moist. The stoma can secrete (make and release) mucus. There is no longer a sphincter muscle that lets you control the passing of stool. The stool will empty into the collection bag on its own. The location of the stoma depends on the area of the colon that was used to create the stoma. The size of the stoma varies.
Your body can still digest food the same way after having a colostomy. There may be changes in stool consistency based on where the stoma is along the colon.
A colostomy may be permanent (life long) or temporary (short term). Your provider will talk to you about your surgery and plan for colostomy.
A colostomy may be done to treat:
- Colon cancer.
- Rectal cancer.
- Some birth defects.
- Diverticulitis.
- Inflammatory bowel disease.
- Colon/rectum injury.
- Bowel obstruction (blockage).
- Perineal fistula/wound.
There are a few different types of colostomy that are separated into three groups. Each group of colostomy refers to a part of the colon. They are:
- Transverse colostomies are in the upper-middle or right abdomen (belly) and include:
- Loop transverse colostomy: Two stomas are made. One to let out stool, the other to let out mucus.
- Double-barrel transverse colostomy: Two stomas are made, one for stool and the other for mucus. The bowel is cut and each end is brought to the surface of the abdomen. The stoma that lets out only mucus is smaller than the one for passing stool. At times, the stoma used to let out mucus is closed, and mucus passes through your anus.
- Ascending colostomy: Not often used. The stool passed from this type of colostomy is liquid and has digestive enzymes in it. This colostomy is in a part of the colon that is earlier in the digestive process, so your body does not have time to break down all of the digestive enzymes.
- Descending and sigmoid colostomies: This colostomy is in the lower left part of the abdomen. The stool that is passed from a descending colostomy is firm. Stool from a sigmoid colostomy is even more solid. Some people may be able to have some control over when they pass stool by eating and drinking certain foods.
What are the risks of having a colostomy?
There are risks and side effects related to having a colostomy. Risks and side effects may be:
- Reaction to anesthesia (Anesthesia is the medication you are given to help you sleep through the surgery, to not remember it and to help with pain. Reactions can include wheezing, rash, swelling and low blood pressure).
- Bleeding.
- Damage to nearby organs.
- Infection.
- Stomal stenosis (narrowing of the stoma opening).
- Adhesion/scar tissue formation (An adhesion is scar tissue that joins 2 pieces of tissue that should not be joined. They are often painless and do not need treatment. Serious cases can cause a blockage in the bowel or limit blood flow).
- Bowel obstruction (This is a blockage in the bowel that can slow or block digestion or the removal of stool).
- Skin irritation at the stoma.
Your care team will talk with you about the risks of your procedure.
What is recovery like?
Recovery from a colostomy depends on the type you had. You may spend a few days in the hospital after the procedure.
You will be told how to care for your surgical incisions (cuts) and stoma. You will be given any other instructions before leaving the hospital, like the need for stomal irrigation (flushing). Full instructions on caring for your stoma will be given to you by a specially trained stoma nurse/therapist.
Your care team will talk with you about the medications you will be taking, like those for pain, blood clot, infection, and constipation prevention and/or other conditions.
Your provider will talk to you about any changes in activity. Often, you should:
- Not lift, bend, or twist until you are told that you can. Ask about when you can start to exercise.
- Not drive while taking pain medication.
- Return to work in 2-4 weeks, based on your job and daily tasks.
- Speak with your healthcare team about showering, putting your surgical incisions under water, diet, sexual activity, and stoma care.
What will I need at home?
- Thermometer to check for fever (101*F/ 38.3*C), which can be a sign of infection. Your care team will tell you at what temperature you should call them.
- Incision and stoma care supplies, often given to you by the hospital, your care team, or the stoma nurse/therapist.
When should I call my provider?
- Signs of infection, such as fever, redness, odor and drainage at your incision.
- Nausea, vomiting, bloating, or cramps lasting more than 2 hours.
- Leg swelling and/or sudden shortness of breath.
- Any new or worsening pain.
- Decrease in how much you are peeing.
- Changes in your stoma including retraction (pulling inward), changes in size or color, stoma blockage or bulging, bleeding, wounds, skin irritation, sores, and/or watery stool for 5 or more hours.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as you are told to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.