Surgical Procedures: Surgery and Staging for Gallbladder Cancer
Table of Contents
What is gallbladder cancer?
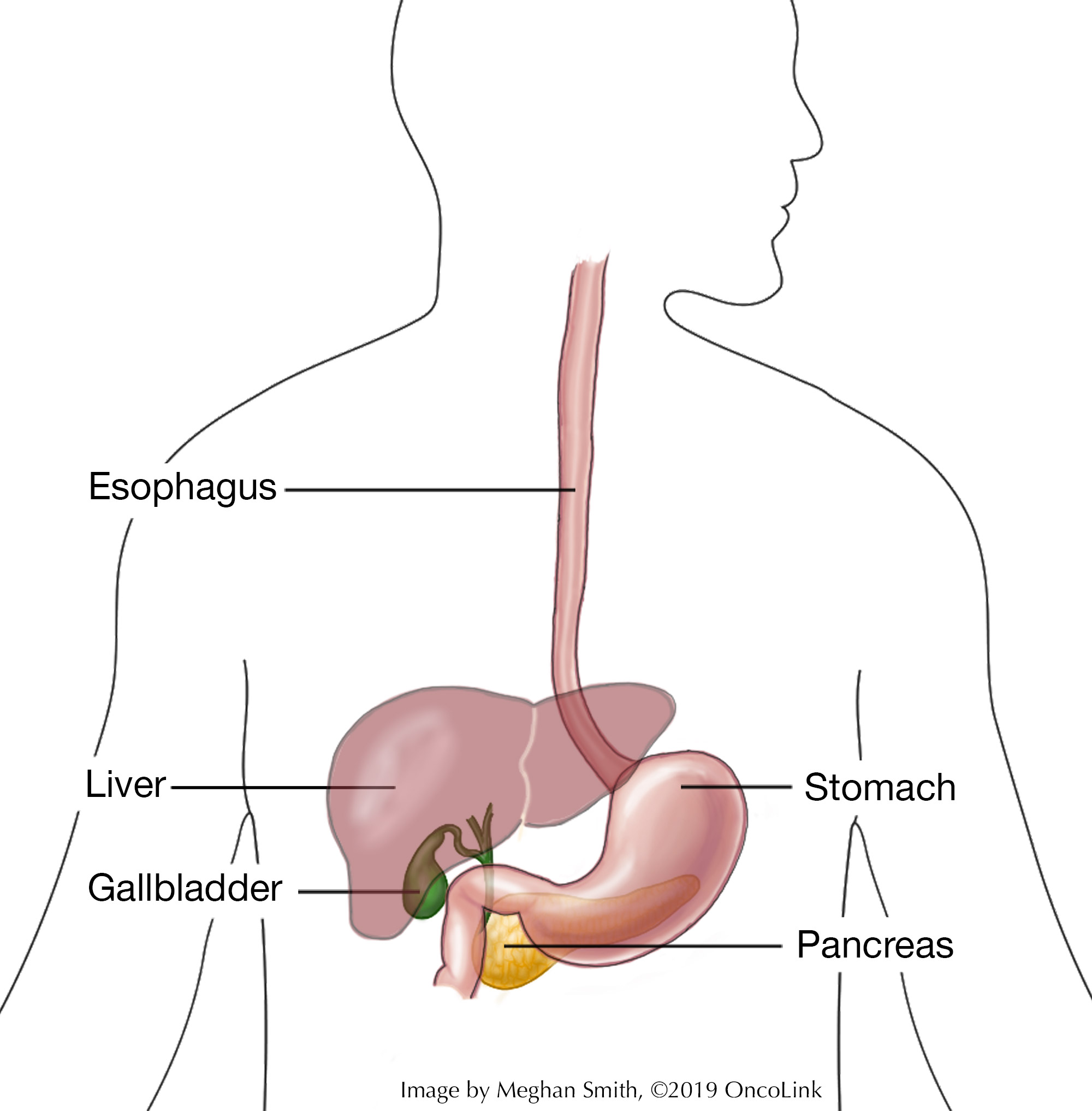
Cancerous cells in the gallbladder are called gallbladder cancer. The gallbladder sits under the liver in the upper right part of your abdomen (belly). It is pear-shaped and stores bile. Bile is a digestive fluid that digests fat. It is made by the liver and stored in the gallbladder until it is ready to be released through the common bile duct of the gallbladder. The common bile duct connects the gallbladder and liver to the first part of the small intestine.
Risk factors are:
- Being female.
- Being of Native American descent.
- Older age.
- Being overweight.
- If you have had gallstones, porcelain gallbladder, choledochal cyst, and chronic gallbladder infection.
Most often, gallbladder cancers start in the inner lining of the gallbladder or mucosa, within the glandular cells. These cancers are classified as adenocarcinoma.
What is staging and how is it done?
Staging is a way to find out if and where the cancer has spread in your body. Your provider will have you get a few tests to figure out the stage of your cancer. These tests may include:
Physical Exam: This is a general exam to look at your body and to talk about your past health issues.
Imaging: Radiology tests can look inside your body at the cancer and see if it has spread. These tests can include:
- Ultrasound.
- Chest X-ray.
- CT scan.
Laboratory Tests: Blood tests such as liver function tests, blood chemistry studies, checking your levels of carcinoembryonic antigen (CEA), and CA 19-9 may be done.
Procedures: Each case of gallbladder cancer is different. Talk with your care team about which procedures may be part of your treatment plan. These options may include:
- Percutaneous Transhepatic Cholangiography (PTC): Dye is put into the liver or bile ducts using a needle that goes into the belly below the ribs. After the dye is put in, an X-ray is taken to look for blockages. Any blockages found may mean stent placement is needed so that bile can drain from the liver. In some cases, bile may need to be drained to a bag outside the body.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): A scope is passed through the mouth, esophagus, and stomach, and it is placed into the first part of the small intestine. Here, a smaller tube is passed through the bile ducts. An X-ray is taken after a dye is put in to look for any blockages. A stent may be placed to keep the duct open.
- Magnetic Resonance Cholangiopancreatography (MRCP): During an MRCP, the liver, gallbladder, bile ducts, pancreas, and pancreatic duct are looked at using a special type of MRI.
- Biopsy: Tissue is removed and looked at under a microscope to check for cancerous cells.
- Laparoscopy: Small incisions (cuts) are made into the abdomen (belly) and the surgeon will use surgical tools in the abdomen to look for cancer, get biopsies, and/or take out organs as needed. This procedure allows the surgeon to see if the gallbladder cancer has metastasized to other areas.
Gallbladder cancer spreads to other parts of the body through the tissue, lymph, and blood systems. Cancer stage tells how extensive the cancer is, how far it has spread, and what treatment course will be suggested. Gallbladder cancer is staged as stage 0 through stage IV. Stage 0 means the cancer is only in the inner layer of the gallbladder. Stage I means the cancer is only in the gallbladder wall. Stages II-IV disease is described as unresectable (unable to be removed with surgery), recurrent (the cancer comes back after treatment or surgery), or metastatic (the cancer has spread in the body). The stage is based on how cancer can be treated.
In some cases, surgery is used to treat gallbladder cancer.
Surgical Procedures for Gallbladder Cancer
There are different surgeries used to treat gallbladder cancer, including curative (removal of the cancer) and palliative (not meant to cure, but to help relieve symptoms). Which surgery you have is based on the stage of your cancer and your situation. These surgical procedures include:
- Staging Laparoscopy: This is done before other surgeries to check for metastasis (spread of cancer) and to see what surgical options there are. During a staging laparoscopy, small incisions (cuts) are made in the belly. Then, a laparoscope (lighted tube) is put in, which lets the surgeon better see the abdomen. At times, if the cancer is thought to be resectable, or operable, then the cancerous areas can be removed during this procedure.
- Simple Cholecystectomy: During this procedure, the gallbladder and some of the surrounding tissue are removed. This is often used for early-stage cancers or non-cancerous diagnoses. Often, gallbladder cancer is found during a procedure for a benign (non-cancerous) condition. There are two ways a simple cholecystectomy can be done:
- Open Cholecystectomy: Removal of the gallbladder through a large abdominal incision. This method is not often used when a patient may have or has cancer. Most patients will have an extended cholecystectomy (see below) in these cases.
- Laparoscopic Cholecystectomy: Small incisions are made within the abdomen, allowing for the placement of a laparoscope (lighted tube) which lets the surgeon better see the abdomen. This method is not used when gallbladder cancer is known or suspected.
- Extended (Radical) Cholecystectomy: Often this is used for patients with gallbladder cancer to lower the risk of disease recurrence. This procedure is the removal of the gallbladder, part of the surrounding liver tissue, and many surrounding lymph nodes. In some cases, a more extensive operation may be needed to remove a larger portion of the liver (wedge resection) or removal of a liver lobe (hepatic lobectomy), the common bile duct, certain ligaments, additional lymph nodes, the pancreas, the duodenum and any other areas where the disease is found.
Palliative (pain and symptom-relieving) procedures include:
- Surgical Biliary Bypass: The gallbladder or bile duct will be cut and attached to the small intestine to allow bile flow, blocked by a tumor, to flow more freely.
- Endoscopic Stent: A stent may be placed in the bile duct to allow bile drainage. This is done when there is a tumor blocking the duct and not allowing the bile to flow freely. In some cases, the bile may drain into the small intestine or outside of the body into a collection bag.
- Percutaneous Transhepatic Biliary Drainage: This procedure is often done if you have jaundice (yellowing of the skin and eyes). During this procedure, a liver and bile duct X-ray is used to see if there are blocked bile ducts. An ultrasound-guided stent is placed to relieve the bile blockage in the small intestine or a collection bag outside the body.
What are the risks of gallbladder surgery?
As with any surgery, there are risks and possible side effects. These can be:
- Reaction to anesthesia (anesthesia is the medication you are given to help you sleep through the surgery, to not remember it, and to manage pain. Reactions can include wheezing, rash, swelling, and low blood pressure).
- Bleeding.
- Blood clots.
- Infection.
- Pneumonia.
- Bile leakage into the abdomen.
- Injury to the bile duct and/or liver.
- Liver failure.
- Scarring and/or incisional numbness.
- Incisional hernia.
- Post-operative digestive problems, such as issues with eating.
What is recovery like?
Recovery from gallbladder cancer surgery will depend on the type of procedure you have had. You may have a tube in your nose that rests in the stomach to remove swallowed air. You may also have drains placed in your surgical wounds.
You will be told how to care for your surgical incision before leaving the hospital.
Your medical team will discuss with you the medications you will be taking, such as those for pain, blood clot prevention and/or other conditions.
Your healthcare provider will tell you if you should change your routine or activity depending on the surgery you have had.
Contact your healthcare team if you experience:
- Fever or chills.
- Abdominal bloating/swelling/cramping/pain.
- Pain that doesn’t get better with medication.
- Nausea or vomiting.
- Incisional drainage, swelling, bleeding, and/or redness.
- Having a hard time eating or drinking.
- Jaundice (yellowing of the skin and/or whites of your eyes).
- 3 days of not passing gas or having a bowel movement.
- Pain located behind the breastbone, shortness of breath, and/or a persistent cough.
- Gray stool.
- Any other concerning symptoms.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you when you can go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.