Brain Tumor, Glioblastoma Multiforme, Frontal Lobe
Case History
History of Present Illness
C.D. is a 62-year-old gentleman who has been in his normal state of health until three weeks ago, when he suddenly started having difficulty with understanding speech and communicating thoughts logically. He also reports progressive inability over the past few weeks to express his thoughts in writing. These symptoms have been severely impeding his ability to perform at work, therefore prompting him to seek medical attention. He denies any recent trauma or history of similar episodes, and is not experiencing other associated symptoms at the moment. However, he later admits that he has been unusually depressed and detached recently.
Past Medical History
Angioplasty three months ago to his left index finger as a cure for a spontaneous hemorrhage
Past Surgical History
Inguinal hernia repair 15 years ago
Medications and Allergies
Denies any outpatient prescription or over-the-counter meds
NKDA
Family History
Negative for heart, lung, kidney disease, diabetes or any cancer.
Negative for mental disability or Alzheimer's disease.
Social History
C.D. is a non-smoker and denies any past or present use of alcohol or illicit drugs. He has worked as a clergyman for most of his adult life and has never been married or fathered any children. He denies recent travel or insect exposures.
Review of Systems
Expressive aphasia, progressive agraphia and depressed mood, as per HPI. He reports no systemic symptoms, although his appetite is decreased. He denies headaches, visual changes, weakness, seizures or loss of consciousness.
Physical Examination
GENERAL: C.D. is a 62-year-old Caucasian male who appears his stated age. He is in no acute distress but has a somewhat depressed affect.
HEENT: pupils are equal, round and reactive to light; extraocular movements are intact; mucus membranes are moist
PULMONARY: lungs are clear to auscultation bilaterally
CARDIOVASCULAR: heart has regular rate and rhythm
ABDOMEN: soft, nontender
EXTREMITIES: no peripheral edema
LYMPH: no peripheral adenopathy palpated
NEURO:
- alert, awake and oriented times three
- speech is slow and labored, with inappropriate word choice and grammar
- cranial nerves II through XII are intact
- muscular strength is 5/5 in all extremities
- sensation and cerebellar function are intact
- reflexes are 2+ bilaterally.
Data
LABS: CBC with differential reveals mild anemia, but otherwise normal. Chemistry panel including LFT's within normal range.
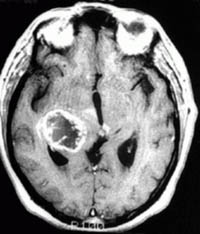
IMAGING: A MRI scan reveals a large left frontal lobe tumor with associated edema. Chest and abdominal CT scans are also obtained and do not demonstrate any additional lesions.
T2 weighted MRI | |
|---|---|
T1 weighted MRI after Gadolinium infusion | |
T2 weighted MRI | T1 weighted MRI after Gadolinium infusion |
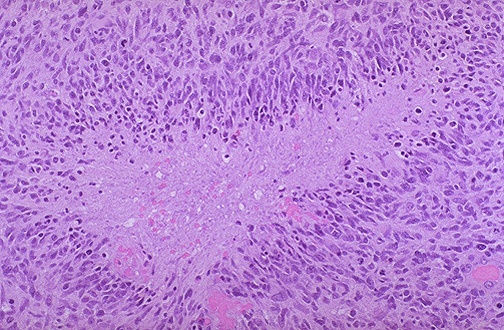
DIAGNOSTIC STUDIES: He undergoes a craniotomy and surgical resection of the tumor without complications. Pathology of the specimen reveals a glioblastoma multiforme, with hyperchromatic, highly pleomorphic cells palisading around areas of alternating necrosis and hypervascularity.
Glioblastoma multiforme, high-power microscopic views (H & E stain) |
|---|
Glioblastoma multiforme, high-power microscopic views (H & E stain) |
Assessment and Plan
C.D. is a 62-year-old Caucasian male with a relatively short course of symptoms prior to his presentation. His development of expressive aphasia and mood disturbances over a relatively brief time period are all worrisome for central nervous system neoplasia. Imaging confirms the presence of a brain tumor, prompting surgery for both diagnostic and therapeutic purposes. Following his craniotomy alone, his memory and speech have improved, although his comprehension remains variable.
Given the pathology of glioblastoma multiforme that was established following surgical resection of the left-sided frontal tumor, he would probably benefit from post-operative radiation therapy to 6000 cGy in approximately 30 fractions. He is also a candidate for the CAI protocol, which is a phase II NABTT study studying CAI, an angiogenesis inhibitor. The risks, benefits and procedures are explained to the patient and his family.
Given the weight of the diagnosis that he has just received today, the patient wishes to think about his options and have further discussion regarding post-operative adjuvant therapy.
Discussion
Glioblastoma multiforme (GBM) and anaplastic astrocytomas are the most common primary brain tumors of adults. The optimal treatment schema includes a maximally safe resection and post-operative radiotherapy. The extent of surgical resection is dictated largely by the location of the tumor. Nondominant frontal lobe tumors can be extensively debulked, whereas tumor in the basal ganglia or thalamus generally can not be as effectively managed.
Treatment with surgery and adjuvant radiation therapy prolongs life but is seldom curative. For patients with glioblastomas, median survival is approximately 10 months, whereas for those with anaplastic astrocytomas, median survival is approximately 2 to 3 years.
With regards to chemotherapy, glioblastomas and anaplastic astrocytomas sometimes respond to BCNU, CCNU, and other nitrosoureas; procarbazine; and the new orally administered alkylating agent temozolomide. These tumors, however, tend to be substantially more resistant to chemotherapy than lymphomas, medulloblastomas, oligodendrogliomas, or germ-cell tumors.
Adjuvant chemotherapy with a nitrosurea or PCV has been shown to increase 1- and 2-year survival rates in patients with GBM or anaplastic astrocytoma by up to 10%. Some believe that anaplastic astrocytomas are more responsive to chemotherapy than are GBMs and recommend adjuvant PCV for young patients with good performance status and intermediate-grade gliomas.
For glioblastoma multiforme, the cure rate is very low with standard local treatment. These patients are appropriate candidates for clinical trials designed to improve local control by adding newer forms of treatment to standard treatment.
Standard Treatment Options:
- Surgery plus radiation therapy and chemotherapy [1, 2]
- Surgery plus radiation therapy.
Under clinical evaluation:
Patients with brain tumors that are either infrequently curable or unresectable should be considered candidates for clinical trials that evaluate the following: hyperfractionated irradiation, accelerated fraction irradiation, stereotactic radiosurgery, radiosensitizers, hyperthermia, interstitial brachytherapy, and intraoperative radiation therapy in conjunction with external-beam radiation therapy. This last technique may be used to improve local control of the tumor and/or for studies that evaluate new drugs and biological response
modifiers following radiation therapy [3, 4, 5, 6]. Cooperative group studies that evaluate hyperfractionated irradiation and interstitial brachytherapy are in progress [7]. Finally, BCNU (carmustine)-impregnated polymer may be implanted during surgery as adjuvant therapy [8,9].