PICC Line
Table of Contents
What is a PICC line?
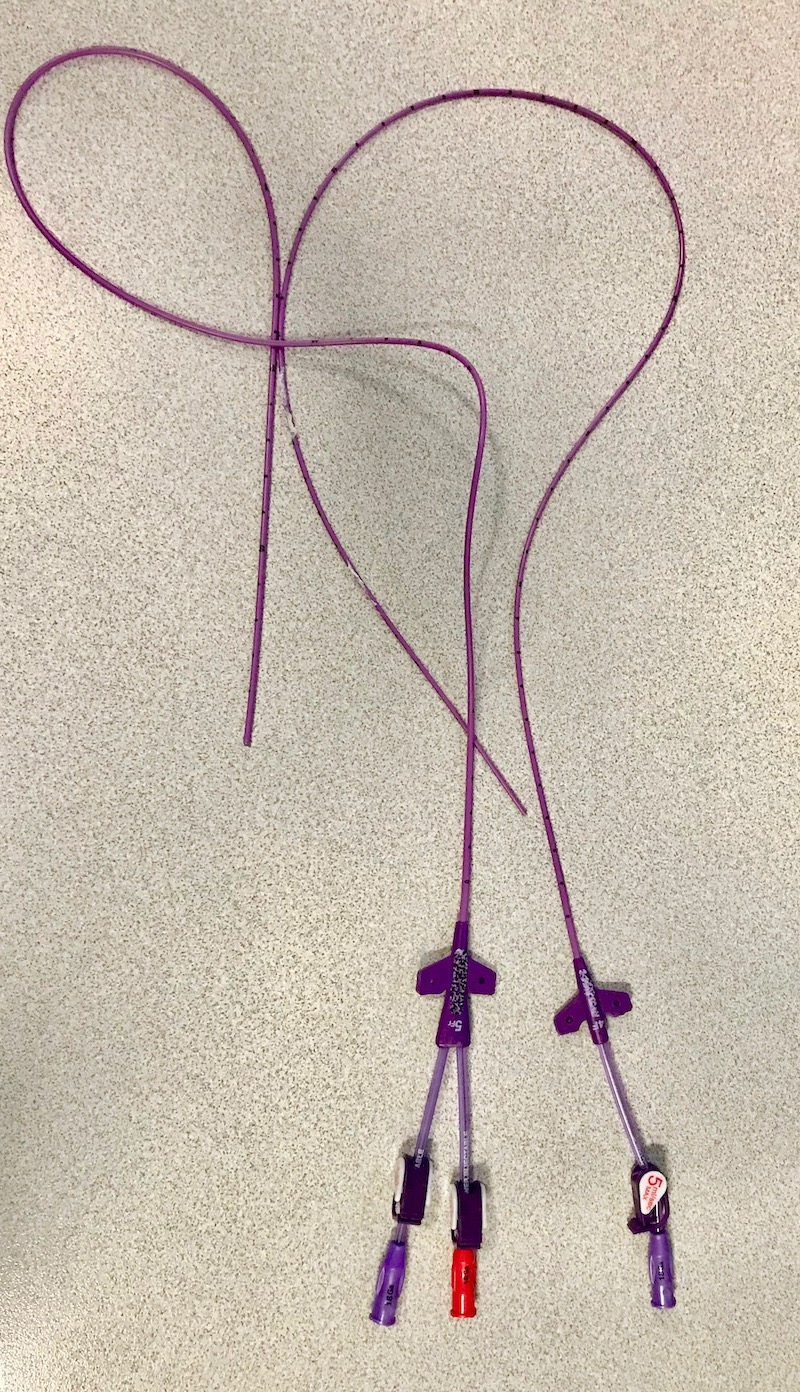
PICC stands for Peripheral Inserted Central Catheter. A PICC line is a long, thin, flexible tube that is put into a vein in your upper arm. The PICC line goes up through the vein in your arm into a larger vein just above your heart. The part of the PICC outside your arm has a cap on it that can be connected to your infusion or a syringe. A PICC line may have 1 to 3 “lines” or “lumens” (tubes) to connect to. They may also be called single, double, or triple lumen catheters. Each lumen can be used to give different things at the same time.
What is a PICC line used for?
A PICC line is used when your veins are hard to put an IV into or you are getting treatments over a period of time. It can stay in for many months. The line can be used for:
- Chemotherapy or other cancer therapies.
- Antibiotics.
- IV fluids.
- Blood products.
- IV nutrition (parental nutrition).
- Taking blood for tests.
How is a PICC line put in?
A PICC line can be put in as an outpatient procedure or while you are already in the hospital. This can be done by a special kind of nurse or by a provider in interventional radiology.
Your provider will use a small ultrasound wand to find your vein. They will get the area ready with sterile drapes and by using a solution to clean and sterilize your arm. Numbing medication will be put into your arm using a small needle. A needle will be put into the vein and the PICC line is threaded through the needle into the vein, then the needle is removed. The area will be covered by a dressing (bandage). The PICC line tubes (lumens) are held in place by either a few stitches or a strong sticker. After the line is put in you will have a chest x-ray to be sure it is in the right place.
What are the risks when getting a PICC line?
Getting a PICC line put in is a safe procedure. There are a few problems that can happen. These are:
- The line could be put in the wrong vein in the body or your provider might not be able to get the tube all the way in. In that case, it can be taken out and a new PICC put back in.
- You could have bleeding from the place it goes into your body.
- In rare cases, the vein could be punctured (a hole put into it) or a nerve in the area could be hurt.
- After the PICC is placed, there is a risk of infection, blood clot, or inflammation in the vein (phlebitis).
- The PICC line can accidentally come out or move out of its position in the vein. Let your provider know if you think the line has moved or come out at all.
- The line can become blocked. Your provider can use a medicine to try to unblock it.
How do I care for my catheter?
- Wash your hands before touching the PICC line. Wear gloves when changing the dressing of the line. After touching the PICC line, wash your hands again.
- Your PICC line will be covered with a dressing. This keeps the area clean and helps keep the PICC line from coming out. The dressing should be changed at least once a week, or if it becomes wet or dirty. The caps on the end of the lumen(s) will also be changed each week.
- Place a plastic cover or sleeve over your PICC line while bathing. Never use scissors to cut away a dressing.
- The PICC line must be flushed regularly so it doesn’t get blocked. To flush the line, first clean the end of the lumen. Then attach a syringe filled with normal saline solution and push the fluid into the PICC line. In some PICC lines, a medication called heparin is also used to prevent clots. Your provider will tell you how often to do this.
- Look at your PICC line each day to check for signs of infection, and that the dressing is clean, dry, and in place. Signs of infection include redness, swelling, any drainage from around the line, pain at the site, or fever (greater than 100.4°F or 38.0°C).
- Do not pull on the PICC line. Be sure to secure the lumens against your skin to prevent them from getting pulled on.
- When your PICC line is no longer needed, it can be removed by your provider in the office. Your care team will show you or a family member how to change the dressing or flush the line if you will need to do this when you are at home.
When to contact your care team
Look at your PICC line every day for any changes. Call your care team right away if you notice any of the following:
- Redness, swelling, any drainage from around the line, pain at the site, or fever (greater than 100.4°F or 38.0°C).
- Swelling or redness in the hand, arm, or chest area up into the neck on the same side as the PICC line.
- If you can’t flush the line.
- If the line comes out of your arm at all or if the lines are cut or broken.
- If you have shortness of breath or tightness in your chest, these can be signs of a serious clot. Go to the nearest emergency room or call 911.
A PICC line needs some care and attention but it can be a useful tool in your cancer treatment. It can save you from having to have multiple IVs and blood draws during your treatment.