Interstitial Brachytherapy for Gynecologic Cancers
Table of Contents
What is brachytherapy?
Brachytherapy is a type of radiation therapy where a source of radiation is put inside your body. A higher dose of radiation is able to reach the area where the tumor is or was before surgery. Brachytherapy for gynecological cancers helps lessen how much radiation your nearby healthy tissues get, like the bowel and bladder. When treating gynecological cancers, brachytherapy may be given along with external beam radiation.
There are two types of brachytherapy used for gynecologic cancers – interstitial and intracavitary. This article will focus on interstitial brachytherapy.
What is interstitial brachytherapy?
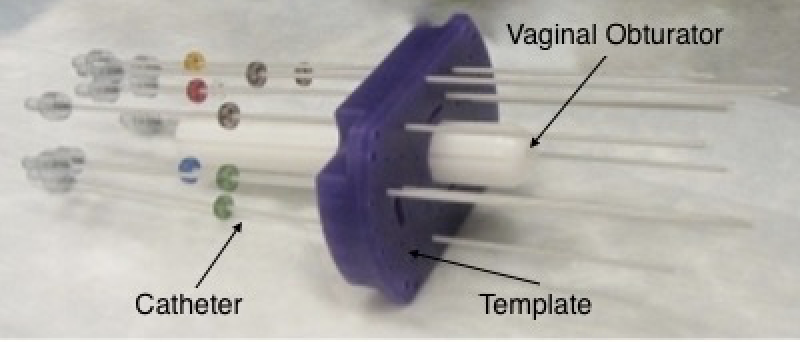
Interstitial brachytherapy uses an applicator that is placed in and close to a tumor, through your vagina or perineum. The applicator has two parts: an obturator and a template. The obturator sits within your vagina. The template is a piece of plastic that is sutured (stitched) to the outside of your body. The template has holes where catheters are put in and kept in a stable position. Interstitial brachytherapy is used for a few reasons:
- The tumor is large.
- The tumor has an odd shape.
- The tumor involves the lower vagina.
- The tumor cannot be reached using intracavitary applicators or the applicators do not fit correctly.
Interstitial brachytherapy is a very specialized type of brachytherapy, and it is specific to each patient's needs.
How is the applicator placed?
The applicator is put into place in the operating room after you have been given general anesthesia (medicine to help you sleep) or an epidural and sedation. A Foley catheter will be placed to collect your urine. A laparoscope, ultrasound, CT, or MRI may be used to help with the placement. Once the applicator is put in place, the template is sutured to your skin. Catheters, or small tubes that look like straws, will be placed through the small holes in the template and into and/or around the tumor on the inside of your body. The applicator, catheters, and Foley catheter will stay in place until you are done with all your radiation treatments. The procedure can be uncomfortable and cause pain. You will be given pain medication. It is important to speak with your provider if your pain is not being controlled.
You will stay on bed rest while the applicator is in place. You will be able to lift the head of your bed to a 20-degree angle. You will not be able to move in bed except for your toes and upper body. You will be given a low residue diet (low in fiber and fat), and in some cases, medications to prevent any bowel movements. You can still have visitors as you are not radioactive.
How is the brachytherapy given?
Treatment often happens 1-2 times per day for a few days. Your provider will talk to you about your treatment schedule. When it is time for your treatment, you will be taken in your bed to the treatment room. A radiation therapist will attach the brachytherapy treatment machine to the catheters in your template. A physicist is also there to take measurements and adjust the catheters if needed. They will make sure everything is in the right position before starting treatment. The physicist will use a tool called a Geiger counter to check the amount of radiation before treatment. The therapist and physicist will then leave the room and the therapist will turn the machine on. The physician is also outside the room monitoring your treatment.
The radioactive source that is in the machine moves into the catheters. Treatment lasts about 10-20 minutes, and the machine may make a clicking sound. You shouldn’t feel any pain during your treatment. Once your treatment is done, the radioactive source moves from the catheters back into the machine. The physicist will use the Geiger counter to make sure that the radiation source is fully back into the machine. The therapist will then disconnect the catheters from the machine.
You will be by yourself in this room as brachytherapy is being given. This is to protect the staff from the effects of the radiation. Make sure that you are comfortable and have no needs before the therapy starts. You will be able to talk with your care team the whole time and if you have any needs during the treatment, you will be able to tell them.
How is the applicator removed?
Once all your treatments are done, you may be given medication to help you relax and possibly sleep. The applicator, catheters, Foley catheter, and any other equipment will be removed. You will likely have some cramping and pain. If your pain is not managed, make sure to tell your provider.
What can I expect after the treatment?
You will stay in the hospital for a few hours or overnight after your last treatment and removal of the applicator. Your provider will tell you how to care for yourself once you go home. Things to keep in mind may include:
- You may have some discharge from your vagina. You can use a pad but not tampons, to help with the discharge. The discharge may be a pinkish color and should not last for longer than a few days.
- You may have cramping, like menstrual cramps, for 24 hours after treatment. You may use ibuprofen (Advil, Motrin or Nuprin) or naproxen (Aleve or Naprosyn) to relieve the cramps. Be sure to follow the instructions on the bottle.
- Some patients have diarrhea. You can take over-the-counter medications, such as loperamide (Imodium) or Kaopectate to help manage any diarrhea. See our managing diarrhea teaching sheet for other tips.
- You will be given vaginal dilators to use once your treatment is done. These will help your vaginal tissue stay flexible, making intercourse more pleasant, but also making pelvic exams more comfortable. You will need to use the dilator for the rest of your life. See our teaching sheet on dilators to learn more about them.
- You are not in any way radioactive after the procedure, and it is safe for friends and family to be around you.
Reasons to call your care team:
- You have a fever. Your care team will tell you at what temperature you should call them.
- You have pain that is not relieved with over-the-counter medication.
- You have a lot of bleeding (more than a menstrual period) or vaginal discharge does not go away.
- You have burning or blood in your urine more than 24 hours after the procedure.
- You do not have a bowel movement for 3-4 days after the procedure.
- You have more than 3-4 episodes of liquid diarrhea a day.
The tools and process used to give interstitial brachytherapy depend greatly on the center where you receive your therapy. Ask your provider about your treatment plan and any questions you have.