Surgical Procedures: Esophagectomy
Table of Contents
What is an esophagectomy and how is it done?
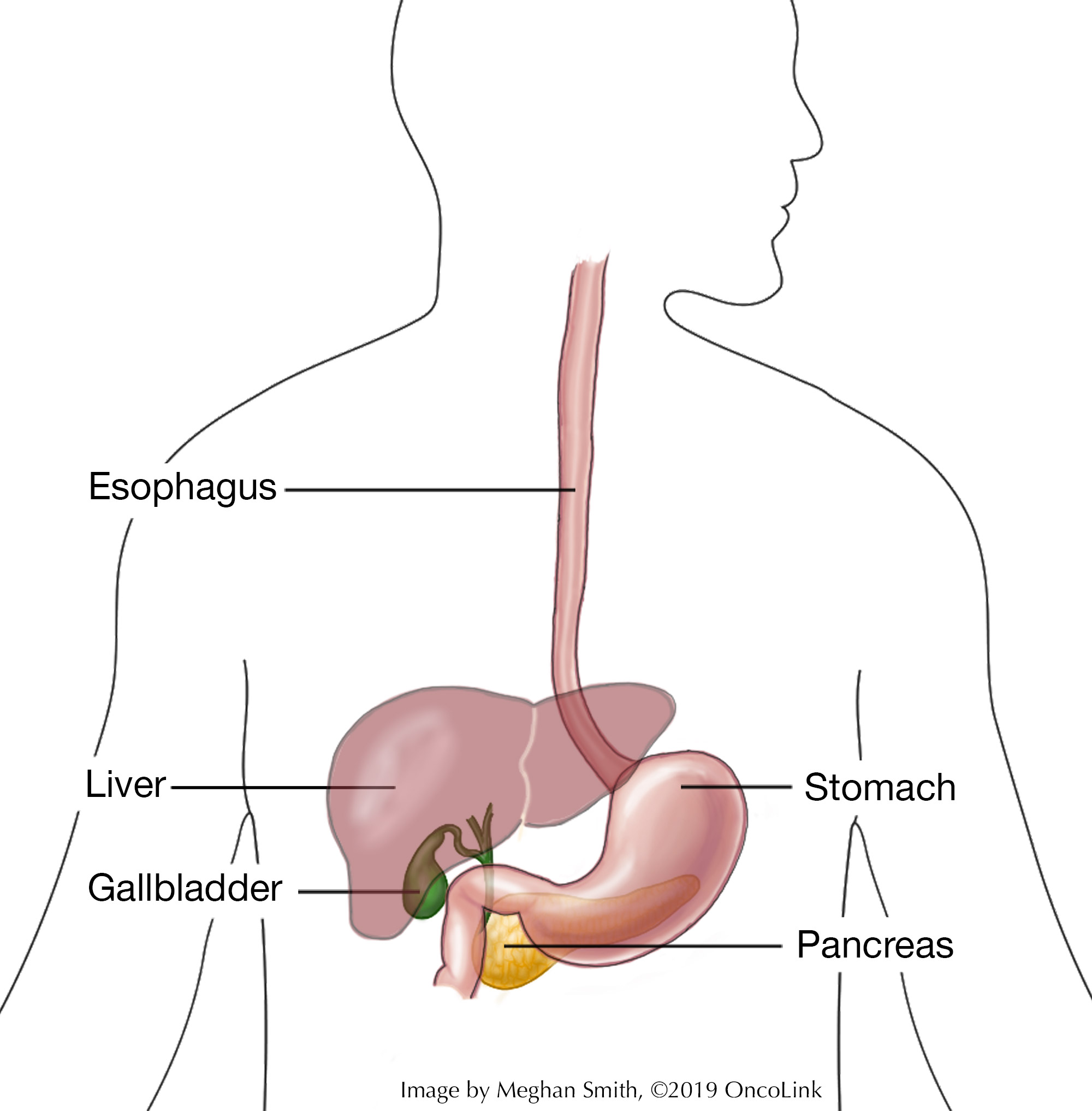
An esophagectomy is surgery to remove part of your esophagus. The esophagus is a tube that connects your throat to your stomach. It helps move food that has been swallowed down to the stomach. There are times when part of your stomach may also need to be removed during an esophagectomy.
An esophagectomy may be used to treat:
- Cancer.
- Barrett’s esophagus.
- Narrowing of the esophagus caused by acid reflux, achalasia (nerve damage to the esophagus), or an injury caused by surgery.
How much of your esophagus is removed depends on many things, like where and how big the tumor is. Sometimes your surgeon will connect your stomach or intestines to a piece of your esophagus that is left in place during surgery.
There are many ways to do an esophagectomy, including:
- Transhiatal (through the diaphragm): Incisions (surgical cuts) are made in your belly and neck.
- Transthoracic (through the thoracic cavity): Incisions are made in your belly and on one side of your chest.
- Thoracoabdominal (through the abdominal cavity): One large incision is made from your chest to your belly.
- Minimally invasive laparoscopic esophagectomy: Many small incisions are made, so that surgical tools and a lighted camera can be used to reach your esophagus.
During any of these types of esophagectomy, lymph nodes may also be removed to check for possible spread of cancer.
What are the risks of an esophagectomy?
There are risks and side effects linked with esophagectomy. Risks and side effects may be:
- Reaction to anesthesia (the medication you are given to help you sleep through the surgery, to not remember it, and to help with pain). Reactions can include wheezing, rash, swelling, and low blood pressure.
- Bleeding.
- Blood clots.
- Injury to your spleen and/or trachea.
- Infection.
- Pneumonia.
- Voice changes.
- Leaking at the site of internal stitches (stitches on the inside of your body) that connect one organ to another. This connection is also called an anastomosis.
- Leaking of a type of lymphatic fluid called chyle.
- Trouble swallowing because of narrowing of the esophagus.
- Delayed gastric emptying (slow digestion).
- Heartburn.
Your surgeon and healthcare team will talk with you about the possible risks of your procedure.
What is recovery like?
Recovery from an esophagectomy depends on the procedure you had. At times, a long hospital stay is needed. During surgery, a feeding tube will be put into your belly and will be used for about 1 to 2 months. This feeding tube will give you nutrition and medication if needed as you heal.
You will be told how to care for your incisions and will be given any other instructions related to your recovery before leaving the hospital.
Your healthcare team will teach you about the medications you will be taking, such as those for pain, and prevention of blood clots, infection, constipation, and/or other conditions.
Your provider will talk to you about changes to your activity level. In general:
- Do not lift heavy objects until told you can do so by your surgical team.
- Rest as needed and do not do any movements that cause pain.
- Hold a pillow over your incisions when coughing or sneezing.
- Avoid tub bathing, hot tubs, and/or swimming pools until your care team says it is okay.
- Change your diet if you are told to do so by your care team.
- Talk with your care team about when it is safe for you to drive, go back to normal activities, and return to work.
What will I need at home?
- A thermometer to check for fever, which can be a sign of infection.
- Wound care supplies, which will likely be given to you when you leave the hospital or in your surgeon’s office.
Call your healthcare provider if you have:
- Fever. Your team will tell you at what temperature you should call them.
- Any new or worsening pain.
- A hard time breathing and/or a cough that doesn’t go away.
- Trouble eating or drinking, or if you have nausea or vomiting after eating.
- Diarrhea or loose bowel movements.
- Yellowing of the skin or whites of your eyes (jaundice).
- Burning in the throat when laying down or during sleep.
- Symptoms of dumping syndrome, such as:
- Stomach cramping.
- Pain in your belly.
- Lightheadedness.
- Dizziness.
- Nausea, and/or diarrhea within 20 minutes of eating.
- Sweating and/or a fast heartbeat.
- Bleeding, warmth, drainage, or redness at the incision.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection, and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.