Surgical Procedures: Surgery and Staging for Esophageal Cancer
Table of Contents
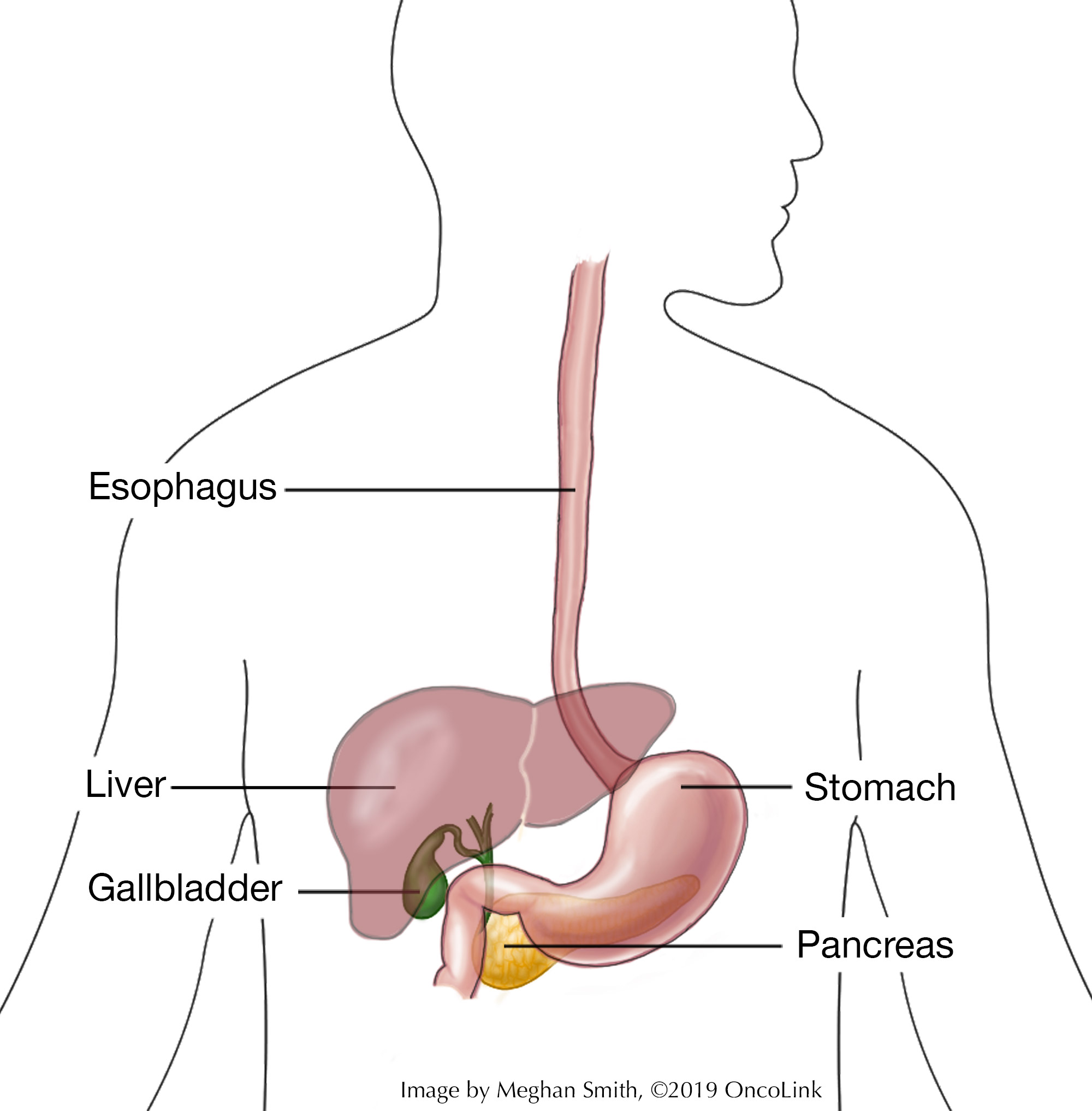
Cancerous cells in the esophagus are called esophageal cancer. The esophagus is found behind the trachea (windpipe). It is a hollow, muscular tube that connects the throat to the stomach. It helps move food from the mouth to the stomach.
Often, esophageal cancers start in the inner lining of the esophagus, or mucosa, and are either squamous cell carcinoma or adenocarcinoma. Other types of esophageal cancers include:
- Lymphomas.
- Melanomas.
- Sarcomas.
- Choriocarcinoma.
- Small cell carcinoma.
What is staging and how is it performed?
Cancer staging determines how extensive the cancer is, how far it has spread, and what treatment can be used. Esophageal cancer can spread to other parts of the body through the tissue, lymph, and blood systems. Your provider will have you get a few tests to figure out the stage of your cancer and if it has spread. For esophagus cancers, these tests may be:
Physical Exam: This is a general exam to look at your body and to talk about past health issues. An oral cavity exam may be done by a provider or dentist.
Imaging: Radiology tests can look inside your body at the cancer and see if it has spread. These tests can include:
- Chest X-Ray.
- CAT scan (CT scan).
- Positron emission tomography scan (PET scan).
- Magnetic resonance imaging (MRI).
- Endoscopic ultrasound (EUS).
Procedures: Each case of esophageal cancer is different. Talk with your care team about which procedures may be part of your treatment plan. These may include:
- Barium Swallow: A barium swallow (upper GI series) uses a barium liquid to coat the esophagus and stomach. The barium helps changes to be seen more clearly. X-rays are then taken to look for any abnormal areas.
- Esophagoscopy: An esophagoscope (a lighted video tube) is put in the mouth or nose and then into the esophagus to look for any changes. Biopsies may be done during the procedure.
- Upper Endoscopy: Similar to the esophagoscopy, but also looks at the stomach.
- Biopsy: A biopsy takes cells from the cancer, or a piece of the cancer, to see what type of cancer it is and how it behaves. A doctor called a pathologist looks at the sample in a laboratory.
Esophageal cancer is described as stages 0 (High-grade dysplasia) through stage IV (4) disease. In addition, grades 1 through 3 describe how abnormal the cancer cells are.
Surgical Procedures to Treat Esophageal Cancer
Surgery is often used to treat esophageal cancers. The procedure you have depends on many things, like the size and location of the cancer, your health, and your goals for care. Your care team will talk to you about your specific procedure.
Surgical procedures used to treat esophageal cancer include:
Esophagectomy: Removal of part or all of the esophagus. Part of the stomach may also be taken out. How much of the esophagus is taken out depends on many factors, including tumor stage and location. At times, the upper portion of the esophagus is connected to the stomach. In this case, part of the stomach acts as the esophagus and is pulled up into the chest or neck area.
In some cases, a stent (a small tube to keep an area open) will be placed in the esophagus to keep it open.
There are two ways to do an esophagectomy:
- Open: A surgeon will make incisions (cuts) in the abdomen (belly) and chest (transthoracic esophagectomy), the abdomen and neck (transhiatal esophagectomy), or through an incision in the neck, chest, and abdomen.
- Minimally Invasive: Many small incisions are made, and a scope (tube with a camera attached to it) and other tools are put into the small incisions. This can be used in some cases of early or small cancers.
Endoscopic Resection: An endoscope (tube with a light and tools attached to it) may be put through the skin or through an opening, such as the mouth, to remove tissue.
Thoroscopy: An incision (cut) is made between the ribs and a lighted video tube is put in to look at the organs in the chest. During the procedure, tissue or lymph node samples and/or removal of part of the lung or esophagus may be done.
Laparoscopy: A laparoscope (tube with a light and tools attached to it) is put through a small belly incision (cut) to look in the abdominal cavity (belly) for cancer. Organs and tissue samples can be taken as well.
After surgery for esophageal cancer, you may need to have a feeding tube placed for nutritional support while you recover.
What are the risks associated with esophageal surgery?
As with any surgery, there are risks and possible side effects. These can be:
- Reaction to anesthesia (anesthesia is the medication you are given to help you sleep through the surgery, to not remember it, and to manage pain). Reactions can include wheezing, rash, swelling, and low blood pressure.
- Pneumonia.
- Bleeding.
- Blood clots.
- Infection.
- Voice changes.
- A leak at the areas where the stomach or intestine connects to the esophagus.
- Narrowing of the esophagus that can lead to trouble swallowing.
- Heartburn, nausea, and/or vomiting.
- Dumping syndrome (when food moves too quickly from the stomach to the small intestine which can cause nausea, feeling of fullness, and diarrhea).
What is recovery like?
Recovery from esophageal cancer surgery will depend on the type of procedure you had. At times, a long hospital stay is needed.
You will be taught how to care for your incisions and feeding tube, if needed, before leaving the hospital. You will learn how to change your diet if needed.
Your medical team will discuss with you the medications you will be taking, such as those for pain and blood clot prevention and/or other conditions.
Your team will talk to you about activity restrictions, which depend on the surgery you had.
Common instructions after an esophagectomy include:
- Do not lift anything heavy.
- Walking often.
- Stop any activity that causes pain.
- When coughing or sneezing, you should press a pillow over any large incisions.
Contact your healthcare team if you experience:
- Fever. Your team will tell you at what temperature they should be contacted.
- Bleeding, redness, warmth, drainage, or other signs of infection at the incision.
- Any new or worsening pain.
- Difficulty breathing and/or a persistent cough (cough that won’t go away).
- Trouble eating or drinking and/or if you are vomiting after meals.
- Diarrhea or loose bowel movements.
- Yellowing of the whites of the eyes (jaundice).
- Throat burning with lying or sleeping.
- Symptoms of dumping syndrome, such as stomach discomfort, cramping, lightheadedness, dizziness, nausea, or diarrhea within 20 minutes of eating a meal, sweating and/or rapid heartbeat.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that you can go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
- Example of a relaxation exercise: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This article contains general information. Please be sure to talk to your care team about your specific plan and recovery.