Vulvar Cancer: Staging and Treatment
Table of Contents
What is staging for cancer?
Staging is the process of learning how much cancer is in your body and where it is. Tests like a gynecological exam (colposcopy and/or vulvoscopy), Pap smear, CT, and MRI may be done to help stage your cancer. Your providers need to know about your cancer and your health so that they can plan the best treatment for you.
Cancer staging looks at the size of the tumor, where it is, and if it has spread to other organs. There are two systems used to stage vulvar cancer:
- American Joint Committee on Cancer.
- FIGO (International Federation of Gynecology and Obstetrics).
They both use the “TNM system” and have three parts:
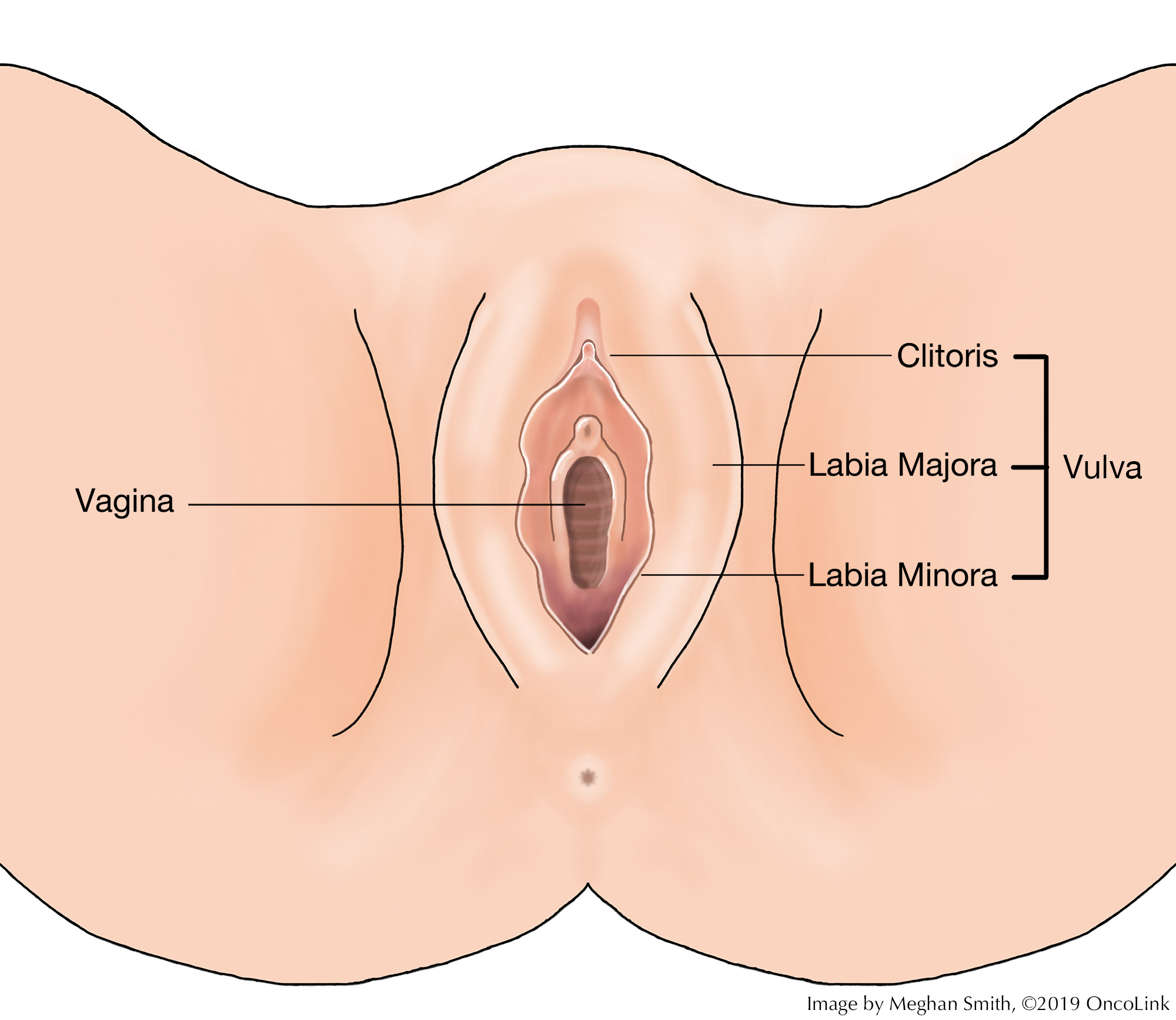
- T-Describes the size/location/extent of the "primary" tumor in the vulva.
- N-Describes if the cancer has spread to the lymph nodes.
- M-Describes if the cancer has spread to other organs (called metastases).
How is vulvar cancer staged?
Staging for vulvar cancer is based on:
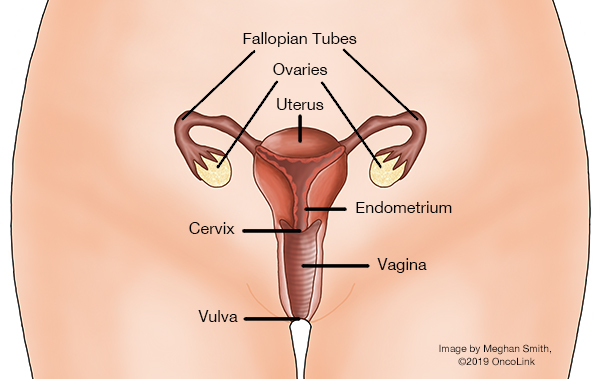
- Where cancer cells are found on gynecological exam/biopsy and if they are in nearby organs or tissue (like the bladder or rectum).
- Surgery or biopsy to test if your lymph nodes have cancer cells.
- Any evidence of spread to other organs (metastasis).
The staging system is very complex. Below is a summary of the staging. Talk to your provider about the stage of your cancer.
Stage IA (T1a, N0, M0): The cancer is in the vulva or the perineum (the space between the rectum and the vagina) or both. It has grown no more than 1 mm (millimeter) into nearby tissue (stroma) and is 2 cm (centimeters) or smaller (about 0.8 inches) (T1a). It has not spread to nearby lymph nodes (N0) or to distant sites (M0).
Stage IB (T1b, N0, M0): The cancer is in the vulva or the perineum or both. It is either more than 2 cm (0.8 inches) or it has grown more than 1 mm (0.04 inches) into nearby tissue (stroma) (T1b). It has not spread to nearby lymph nodes (N0) or to distant sites (M0).
Stage II (T2, N0, M0): The cancer can be any size. It is growing into the anus or the lower part of the vagina or urethra (the tube that drains urine from the bladder) (T2). It has not spread to nearby lymph nodes (N0) or to distant sites (M0).
Stage IIIA (T1 or T2, N1, M0): Cancer is in the vulva or perineum or both (T1). It may be growing into the anus, lower vagina, or lower urethra (T2). It has either spread to one nearby lymph node with the area of cancer spread 5 mm or more, OR it has spread to 1 or 2 nearby lymph nodes with both areas of cancer spread less than 5 mm (N1). It has not spread to distant sites (M0).
Stage IIIB (T1 or T2, N2a or N2b, M0): Cancer is in the vulva or perineum or both (T1). It may be growing into the anus, lower vagina, or lower urethra (T2). The cancer has spread either to 3 or more nearby lymph nodes, with all areas of cancer spread less than 5 mm (N2a); OR the cancer has spread to 2 or more lymph nodes with each area of spread 5 mm or greater (N2b). It has not spread to distant sites (M0).
Stage IIIC (T1 or T2, N2c, M0): Cancer is in the vulva or perineum or both (T1). It may be growing into the anus, lower vagina, or lower urethra (T2). The cancer has spread to nearby lymph nodes and has started growing through the outer covering of at least one of the lymph nodes (called extracapsular spread; N2c). It has not spread to distant sites (M0).
Stage IVA (T1 or T2, N3, M0; T3, Any N, M0): Cancer is in the vulva or perineum or both (T1). It may be growing into the anus, lower vagina, or lower urethra (T2). The cancer has spread to nearby lymph nodes and has become stuck (fixed) to the underlying tissue or has caused an ulcer(s) to form on the lymph node(s)(N3). It has not spread to distant sites (M0); OR the cancer has spread beyond nearby tissues to the bladder, rectum, pelvic bone, or upper part of the urethra or vagina (T3). It may or may not have spread to nearby lymph nodes (any N). It has not spread to distant sites (M0).
Stage IVB (Any T, Any N, M1): The cancer has spread to distant lymph nodes (pelvic) or organs such as lung or bone (M1). The cancer can be any size and may or maynot have spread to nearby organs (Any T). It might or might not have spread to nearby lymph nodes (Any N).
How is vulvar cancer treated?
Treatment for vulvar cancer depends on where your cancer is and if it has spread. For pre-cancers (vulvar intraepithelial neoplasia or VIN), topical therapy may be used. Topical therapy means a cream or ointment that is put on the skin. For vulvar cancer, your treatment may include some or all of the following:
Surgery
The goal of surgery is to remove all or as much of the cancer as possible while trying to keep other tissue and organs safe. Your surgeon will also try to leave you with as much normal sexual function as possible after surgery. There are a few surgical options to treat cancer of the vulva:
- Laser surgery: A laser beam burns off the layer of vulvar skin that has cancer cells in it. This type of surgery is only used for pre-cancers and not invasive cancer.
- Excision: The cancer and a small area of normal skin (called the margin) is excised (cut out). If a lot of skin is removed, it is called a simple partial vulvectomy.
- Vulvectomy:
- Skinning vulvectomy: Only the top layer of skin that has cancer in it is removed.
- Simple vulvectomy: The whole vulva is removed, as well as tissue just under the skin’s surface.
- Partial or modified radical vulvectomy: Part of the vulva is removed with some deep tissue.
- Complete radical vulvectomy: The whole vulva and deep tissue are removed.
- Vulvar reconstruction: If you have had a lot of skin removed from the vulva, you may need skin grafts from another part of the body to cover the wound. A skilled plastic/reconstructive surgeon will do this surgery if needed.
- Pelvic exenteration: This surgery is a complete radical vulvectomy, removal of pelvic lymph nodes, and the removal of at least one of the following: the lower colon, rectum, bladder, cervix, uterus, and vagina. What is removed depends on where the cancer is. Talk with your surgeon about what will be removed during your surgery.
Radiation
Radiation therapy is the use of high-energy x-rays to kill cancer cells. Radiation can be used:
- With chemotherapy to treat vulvar cancer (chemoradiation).
- Before surgery, to shrink the tumor so that it is easier to remove during surgery.
- After surgery to kill any cancer cells that may have been left in your body.
- If you are not well enough to have surgery.
Chemotherapy
Chemotherapy is the use of anti-cancer medications to kill cancer cells. Chemotherapy may be given with radiation therapy before surgery. There are no standard chemotherapy treatment plans, but these medications may be used:
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Service.
Making Treatment Decisions
Your care team will make sure you are included in choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It feels like an emergency, but you can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot make the decision for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
You can learn more about vulvar cancer at OncoLink.org.