Nasopharyngeal (Upper Throat) Cancer: Staging and Treatment
Table of Contents
What is staging for cancer?
Staging is the process of learning how much cancer is in your body and where it is. Tests like biopsy, nasopharyngoscopy, bone scan, PET scan, CT, and MRI may be done to help stage your cancer. Your providers need to know about your cancer and your health so that they can plan the best treatment for you.
Cancer staging looks at the size of the tumor and where it is, and if it has spread to other areas of your body. The staging system for nasopharyngeal cancer is called the “TNM system.” It has three parts:
- T-Describes the size/location/extent of the "primary" tumor.
- N-Describes if the cancer has spread to the lymph nodes.
- M-Describes if the cancer has spread to other organs (called metastases).
Your healthcare provider will use the results of the tests you had to determine your TNM result and combine these to get a stage from 0 (zero) to IV (four).
How is nasopharyngeal cancer staged?
Staging for nasopharyngeal (upper throat) cancer is based on:
- The size of your tumor seen on imaging tests and what is found after surgery (if you have had surgery).
- If your lymph nodes have cancer cells in them.
- If the cancer has spread to other parts of your body (metastasis).
The staging system is very complex. Below is a summary of the staging. Talk to your provider about the stage of your cancer.
Stage 0 (Tis, N0, M0): The tumor is only in the top layer of cells lining the inside of the nasopharynx and has not grown any deeper (Tis). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0).
Stage I (T1, N0, M0): The tumor is in the nasopharynx. It may have grown into the oropharynx (the part of the throat in the back of the mouth) and/or nasal cavity but no farther (T1). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0).
Stage II (T0-T1, N1, M0): The tumor is in the nasopharynx. It may have grown into the oropharynx (the part of the throat behind the mouth) and/or nasal cavity but no farther (T1), OR No tumor is seen in the nasopharynx, but cancer is found in lymph nodes in the neck and is positive for Epstein-Barr virus (EBV) DNA, which makes it very likely to be NPC (T0). The cancer has spread to 1 or more lymph nodes on one side of the neck, or it has spread to lymph nodes behind the throat. In either case, no lymph node is larger than 6 cm (N1). The cancer has not spread to distant parts of the body (M0); OR (T2, N0-N1, M0): The tumor has grown into the tissues of the left or right sides of the upper part of the throat, but not into bone (T2). The cancer has not spread to nearby lymph nodes (N0), OR it has spread to 1 or more lymph nodes on one side of the neck, or it has spread to lymph nodes behind the throat. In either case, no lymph node is larger than 6 cm (N1). The cancer has not spread to distant parts of the body (M0).
Stage III (T0-T1, N2, M0): The tumor is in the nasopharynx. It may have grown into the oropharynx (the part of the throat behind the mouth) and/or nasal cavity but no farther (T1), OR No tumor is seen in the nasopharynx, but cancer is found in lymph nodes in the neck and is positive for Epstein-Barr virus (EBV) DNA, which makes it very likely to be NPC (T0). The cancer has spread to lymph nodes on both sides of the neck, which are not larger than 6 cm (N2). The cancer has not spread to distant parts of the body (M0); OR (T2, N2, M0): The tumor is in the tissue on the left or right sides of the upper throat, but not in the bone (T2). The cancer has spread to lymph nodes on both sides of the neck, which are not larger than 6 cm (N2). The cancer has not spread to distant parts of the body (M0); OR (T3, N0-N2, M0): The tumor has grown into the sinuses and/or the bones nearby (T3). The cancer may or may not have spread to nearby lymph nodes in the neck or behind the throat, but they are not larger than 6 cm (N0 to N2). The cancer has not spread to distant parts of the body (M0).
Stage IVA (T4, N0-N2, M0): The tumor has grown into the skull and/or cranial nerves, the hypopharynx (lower part of the throat), the main salivary gland, or the eye or its nearby tissues (T4). The cancer may or may not have spread to nearby lymph nodes in the neck or behind the throat, but they are not larger than 6 cm (N0 to N2). The cancer has not spread to distant parts of the body (M0); OR (Any T, N3, M0): The tumor might or might not have grown into structures outside the nasopharynx (any T). The cancer has spread to lymph nodes that are either larger than 6 cm or located in the shoulder area just above the collarbone (N3). The cancer has not spread to distant parts of the body (M0).
Stage IVB (Any T, Any N, M1): The tumor may or may not have grown into structures outside the nasopharynx (any T). The cancer may or may not have spread to nearby lymph nodes (any N). The cancer has spread to distant parts of the body (M1).
How is nasopharyngeal cancer treated?
Treatment for nasopharyngeal cancer is based on things like your cancer stage, age, overall health, and testing results. There are steps to take before you start treatment for any kind of head and neck cancer:
- Multidisciplinary treatment is very important. This means you will have providers from many different specialties involved in your care. Many of these providers will see you before you start cancer treatment during visits called consultations. They will work together and with you to create a plan to treat your cancer.
- If you smoke, quit as soon as possible. Smoking may lessen how well your cancer medications work and can make side effects worse.
Your treatment may include some or all the following:
- Surgery
- Radiation Therapy.
- Chemotherapy.
- Targeted Therapy.
- Immunotherapy.
- Supportive/Palliative Treatment.
- Clinical Trials.
Surgery
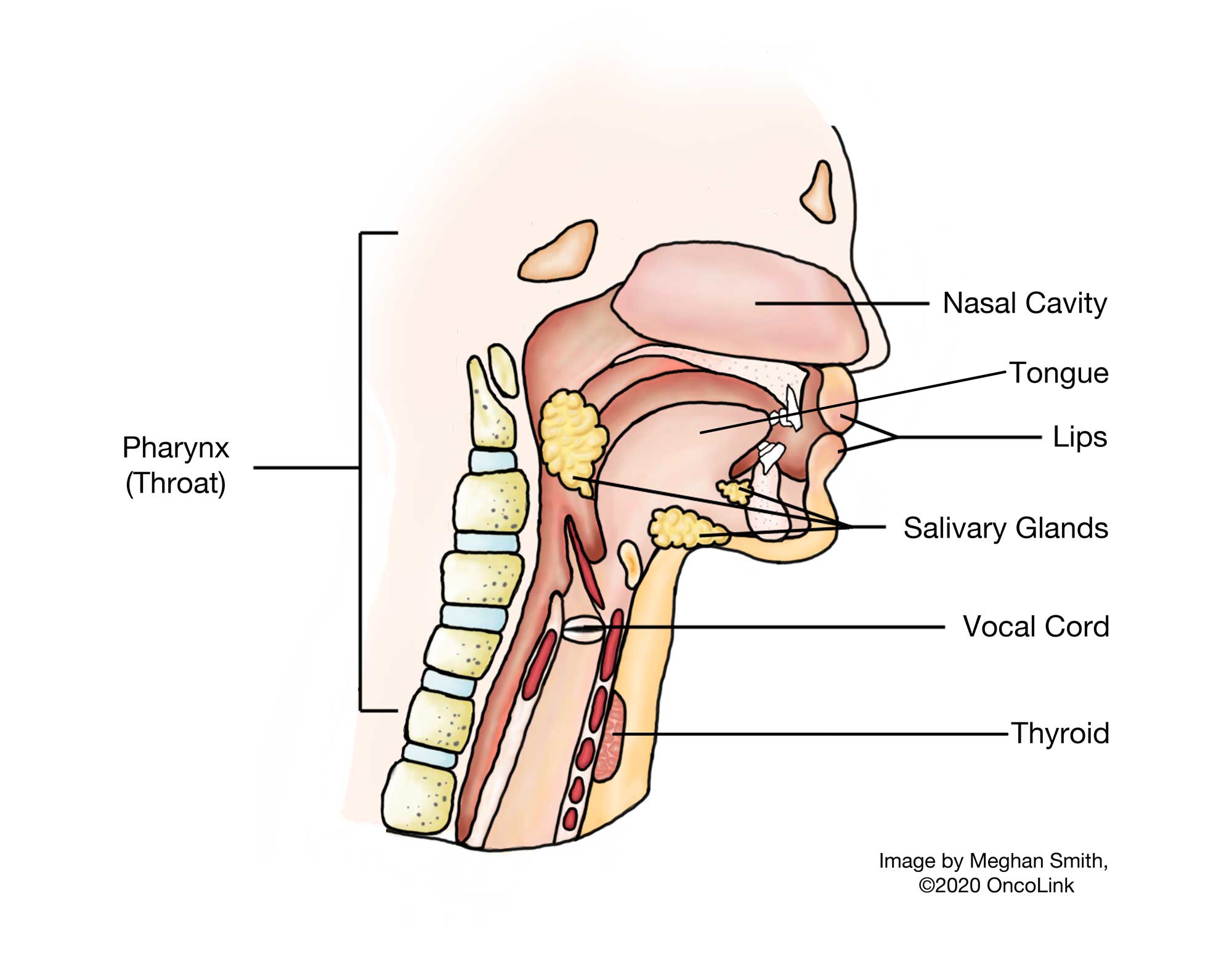
The type of surgery you have depends on where your tumor is, the stage, and your overall health. Surgery for head and neck cancer can be challenging, including the removal of tissue and bone and the use of plastic surgery to rebuild facial features to improve how they work and look. The surgery used most often for nasopharyngeal cancer is called an endoscopic nasopharyngectomy. A flexible scope with a camera and long, thin tools go in through the nostrils to the nasal cavity to remove as much of the tumor as possible.
Talk with your care team about surgical options you have, any concerns about your body image and function, what you will need to do to heal after surgery, and side effects that you may have.
Radiation Therapy
Radiation therapy is the use of high-energy x-rays to kill cancer cells. Radiation for nasopharyngeal cancer can be used:
- Alone.
- With chemotherapy at the same time (called chemoradiation).
- After chemotherapy.
- For palliative treatment (to ease symptoms).
- If the cancer has come back (recurrence).
There are two main types of radiation used to treat nasopharyngeal cancer:
- External radiation therapy: A beam of radiation from outside of the body is directed into the body. It may also be called x-ray therapy, 3D conformal radiation, intensity-modulated radiation therapy (IMRT), cobalt, photon, or proton therapy. When this type of radiation is used, you will likely need to wear a mask that is fitted for you to help you keep still during treatments. This mask can cause anxiety and claustrophobia. Your providers will be able to give you advice to help you with wearing the mask during treatment.
- Internal radiation therapy: A radioactive source is placed inside the body, in or near the tumor. This is called brachytherapy or implant therapy. This type of radiation is often only used when oral cavity, lip, and oropharyngeal cancer has come back.
Because radiation can affect nearby tissues, there are many potential side effects of radiation for head and neck cancers. Talk with your care team about which type of radiation, if any, you will have and the side effects that may happen.
Chemotherapy
Chemotherapy is the use of anti-cancer medications to kill cancer cells. It can be used with radiation therapy (chemoradiation), as the first treatment before chemoradiation, after radiation therapy (called adjuvant chemotherapy), to help with symptoms (called palliative therapy), or to treat cancer that has come back (recurrence).
Chemotherapy medications that may be used are cisplatin, 5-fluorouracil (5-FU), gemcitabine, carboplatin, epirubicin, paclitaxel, docetaxel, capecitabine, and methotrexate. These medications can cause side effects. Ask your medical oncologist which medications would be best for you and when during treatment you will receive them.
Targeted Therapy
Nasopharyngeal cancer may be treated with targeted therapies that focus on specific gene mutations or proteins in the tumor. Targeted therapies work by targeting something specific to a cancer cell, which lets the medication kill cancer cells and affect healthy cells less. Sometimes the “target” is found on a certain type of healthy cell and side effects can happen as a result. An example of a targeted therapy used for this type of cancer is cetuximab.
Immunotherapy
Immunotherapy is the use of a person's own immune system to kill cancer cells. Immunotherapy medications that may be used to treat this type of cancer are toripalimab-tpzi, pembrolizumab and nivolumab.
Supportive/Palliative Treatment
Your quality of life is very important during and after treatment for head and neck cancer. Supportive and palliative treatments are used to lessen symptoms or side effects that you may have. Head and neck cancer treatment and the cancer itself can cause:
- Pain: Your care team will help you with medications and other therapies for pain. Radiation, surgery, and a nerve block can help as well.
- Nutrition issues: For some patients, difficulty swallowing, mucositis (sore mouth and throat), loss of taste, or a lack of saliva production may make eating hard or impossible. It is important that you are followed closely by a dietitian to support you in food and supplement choices, and to keep good nutritional status. If needed, a speech and swallowing specialist can test if you can swallow safely without choking or inhaling food. Many patients will need to be fed through a tube placed in their stomach (called a PEG or ‘G' tube). In most cases, this is only temporary (for a short time).
- Changes in Body Image: Social workers and psychologists may be needed to help in dealing with the changes in body image and your role in your family.
- Speech problems: A speech therapist can help you regain as much of your speech as possible, and also give you other ways to communicate.
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Service.
Making Treatment Decisions
Your care team will make sure you are included in choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It feels like an emergency, but you can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot make the decision for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
You can learn more about head and neck cancers at OncoLink.org.