Thyroid Cancer: Staging and Treatment
Table of Contents
What is staging for cancer?
Staging is the process of learning how much cancer is in your body and where it is. Tests like thyroid scan, thyroid ultrasound, fine-needle aspiration biopsy, CT, and MRI may be done to help stage your cancer. Your providers need to know about your cancer and your health so that they can plan the best treatment for you.
Cancer staging looks at the size of the tumor and where it is, and if it has spread to other organs. The staging system for thyroid cancer is called the “TNM system.” It has three parts:
- T-Describes the size/location/extent of the "primary" tumor in the thyroid.
- N-Describes if the cancer has spread to the lymph nodes.
- M-Describes if the cancer has spread to other organs (called metastases).
How is thyroid cancer staged?
Staging for thyroid cancer is based on:
- The size of your tumor seen on imaging tests and what is found after surgery.
- If your lymph nodes have cancer cells in them.
- If the cancer has spread to other organs (metastasis).
- Your age.
The staging system is very complex. Below is a summary of the staging. Talk to your provider about the stage of your cancer.
Differentiated (papillary or follicular) thyroid cancer
People who are younger than 55 years old and do not have distant spread (metastasis) are always considered Stage I. All patients who are younger than 55 years old and have distant spread of the cancer are considered Stage II. Staging for people of all ages is listed below:
Stage I
- Younger than 55 (Any T, any N, M0): The cancer is any size (Any T) and may or may not have spread to nearby lymph nodes (Any N). It has not spread to distant sites (M0).
- Older than 55:
- (T1, N0/NX, M0): The cancer is no larger than 2 centimeters (cm) (0.8 inches) wide and is confined to the thyroid (T1); OR
- (T2, N0/NX, M0): The cancer is larger than 2 cm. (0.8 inches) wide but no larger than 4cm and is confined to the thyroid (T2). It has not spread to nearby lymph nodes (N0) or to distant sites (M0).
Stage II
- Younger than 55: (Any T, Any N, M1). The cancer is any size (Any T). It may or may not have spread to nearby lymph nodes (Any N). It has spread to other parts of the body, like distant lymph nodes, internal organs, bones, etc. (M1).
- Older than 55:
- (T1, N1, M0): The cancer is no larger than 2 cm. (0.8 inches) wide and is confined to the thyroid (T1). It has spread to nearby lymph nodes (N1). It has not spread to distant sites (M0).
- (T2, N1, M0): The cancer is larger than 2 cm. (0.8 inches) wide but no larger than 4cm and is confined to the thyroid (T2). It has spread to nearby lymph nodes (N1). It has not spread to distant sites (M0).
- (T3a or 3b, Any N, M0): The cancer is larger than 4 cm. but is confined to the thyroid (T3a) or it has grown into the strap muscles around the thyroid (T3b). It may or may not have spread to nearby lymph nodes (Any N). It has not spread to distant sites (M0).
Stage III
- Older than 55: (T4a, Any N, M0): The cancer is any size and has grown beyond the thyroid gland into nearby tissues of the neck, like the larynx (voice box), trachea (windpipe), esophagus (tube that connects the throat to the stomach), or the nerve to the larynx (t4a).
Stage IVA
- Older than 55: (T4b, Any N, M0): The cancer is any size and has grown beyond the thyroid gland back toward the spine or into nearby large blood vessels (T4b). It may or may not have spread to nearby lymph nodes (Any N). It has not spread to distant sites (M0).
Stage IVB
- Older than 55: (Any T, Any N, M1): The cancer is any size (Any T) and may or may not have spread to nearby lymph nodes (Any N). It has spread to other parts of the body, like distant lymph nodes, internal organs, bones, etc. (M1).
Anaplastic (undifferentiated) thyroid cancer
All anaplastic thyroid cancers are considered stage IV. The different groupings for stage IV are listed below.
Stage IVA (T1, T2, or T3, N0 or NX, M0): The cancer is any size and has been confined to the thyroid (T1, T2, T3). It has not spread to nearby lymph nodes (N0, NX). It has not spread to distant sites (M0).
Stage IVB (T1, T2, or T3a, N1, M0; OR T3b, Any N, M0; OR T4, Any N, M0): The cancer is any size and has been confined to the thyroid (T1, T2, T3), has grown into the strap muscles around the thyroid (T3b), or has grown beyond the thyroid gland into nearby tissue of the neck, like the larynx, trachea, esophagus, toward the spine, or into nearby large blood vessels (T4). It may or may not have spread to nearby lymph nodes (Any N, N1). It has not spread to distant sites (M0).
Stage IVC (Any T, Any N, M1): The cancer is any size (Any T) and may or may not have spread to nearby lymph nodes (Any N). It has spread to other parts of the body, like distant lymph nodes, internal organs, bones, etc. (M1).
How is thyroid cancer treated?
Treatment for thyroid cancer depends on many things, like your cancer stage, age, overall health, and testing results. Your treatment may include some or all these:
- Surgery.
- Supplemental thyroid hormone therapy.
- Radioactive iodine therapy.
- Radiation therapy.
- Chemotherapy/ targeted therapy.
- Clinical trials.
Surgery
The goal of thyroid cancer surgery is to remove the tumor. There are a few ways to do so:
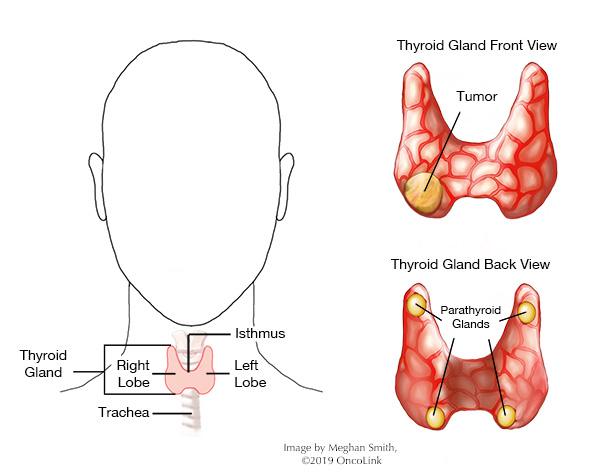
- Total thyroidectomy-The whole thyroid gland is removed.
- Near-total thyroidectomy- Only a small part of thyroid tissue is left. The parathyroid glands are also left, which are attached to the thyroid.
- Lobectomy- A single lobe of the thyroid gland is removed. For patients with small (less than 1 cm.) papillary thyroid cancers, a lobectomy may be used.
If the thyroid is not completely removed during surgery, there may be a risk of the cancer coming back (recurring) in the part of the thyroid that is left. More surgery may be needed to remove the rest of the thyroid if it wasn’t removed during the first surgery.
If your provider thinks you may have thyroid cancer, you should also have an ultrasound of your lymph nodes done. If the cancer has spread to the lymph nodes, your surgeon will also remove these lymph nodes during surgery. Depending on the staging of your cancer, you may need more treatment after surgery.
Supplemental thyroid hormone therapy
Since all or most of your thyroid is gone, you will need to replace the thyroid hormone the gland had made. This is done with medications and is called “supplemental thyroid hormone therapy.” Thyroid hormone can also act as cancer therapy. You may be given slightly more thyroid hormone than what your body would normally make. This helps keep any leftover thyroid cancer inactive (or asleep). In other words, if your body finds that thyroid hormone is already there (through supplemental thyroid hormone therapy), it will not send signals for your thyroid to “turn on.”
Radioactive iodine therapy (RAI)
Thyroid tissue and some thyroid cancers take up iodine into their cells. Radioactive iodine therapy (RAI) uses radioactive iodine, I-131, (RAI) to kill thyroid cancer cells (called "remnant" ablation). Your provider may use RAI if your tumor has a higher risk of coming back or has come back (recurrence), such as tumors that:
- Are bigger than 2 cm.
- Have grown through the thyroid capsule or into the soft tissues of the neck.
- Have spread to the lymph nodes or other parts of the body.
- Have come back (recurrence).
RAI can be an effective therapy in many cases, but some thyroid cancers do not take up iodine. In those cases, RAI will not be helpful.
How RAI Works
The iodine is taken up into the cell and the radiation that is in the radioactive iodine is released, giving a dose of radiation that kills nearby cells. This treatment works well because only the thyroid cells take up and retain (keep) iodine, so other tissues are not often affected. For the first few days after treatment with RAI, you give off radiation and should not be in close contact with others.
Risks of RAI
Research has shown RAI may raise the risk of getting myelodysplastic syndromes (MDS), which can lead to blood cancer. The risk of MDS is higher within the first two years of RAI treatment. Patients and their care teams should look at the risks of treating low risk, well-differentiated thyroid cancers with RAI. The American Thyroid Association guidelines for treatment do not support the treatment of low-risk thyroid tumors with RAI.
Radiation Therapy
Radiation treatment is the use of high-energy x-rays to kill cancer cells. Radiation therapy can be helpful if you have an aggressive type of thyroid cancer, a high risk of recurrence, or have residual (leftover) disease after surgery. High-risk thyroid cancers include incomplete resection (not being able to remove the whole thyroid/tumor), spread outside the thyroid gland to soft tissues of the neck or to regional lymph nodes, some histological subtypes of thyroid cancer, and those cancers that do not take up RAI. It is also used in many cases of anaplastic thyroid cancer to try to stop or slow down the cancer.
Chemotherapy/Targeted therapy
Chemotherapy is the use of anti-cancer medications to kill cancer cells. Chemotherapy is not often used in the treatment of thyroid cancer. However, chemotherapy drugs like paclitaxel, doxorubicin, cisplatin, and carboplatin may sometimes be used in the treatment of metastatic disease (cancer that has spread), anaplastic thyroid cancers, or disease that has progressed after RAI or radiation therapy. Doxorubicin, fluorouracil, and dacarbazine, in combination, may be used in the treatment of medullary thyroid cancer. In anaplastic thyroid cancers, dabrafenib, trametinib, entrectinib, and selpercatinib are used.
A few types of targeted therapy can be used in the treatment of certain thyroid cancers. These medications target specific mutations in cancer cells. Your tumor will be tested for these mutations. These medications include vandetanib, cabozantinib, larotrectinib, entrectinib, selpercatinib, lenvatinib, sorafenib, sunitinib, axitinib, everolimus, pazopanib, dabrafenib and trametinib.
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Services.
Making Treatment Decisions
Your care team will make sure you are included in choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It feels like an emergency, but you can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot make the decision for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
You can learn more about thyroid cancer at OncoLink.org.