Surgical Procedures: Surgery and Staging for Rectal Cancer
Table of Contents
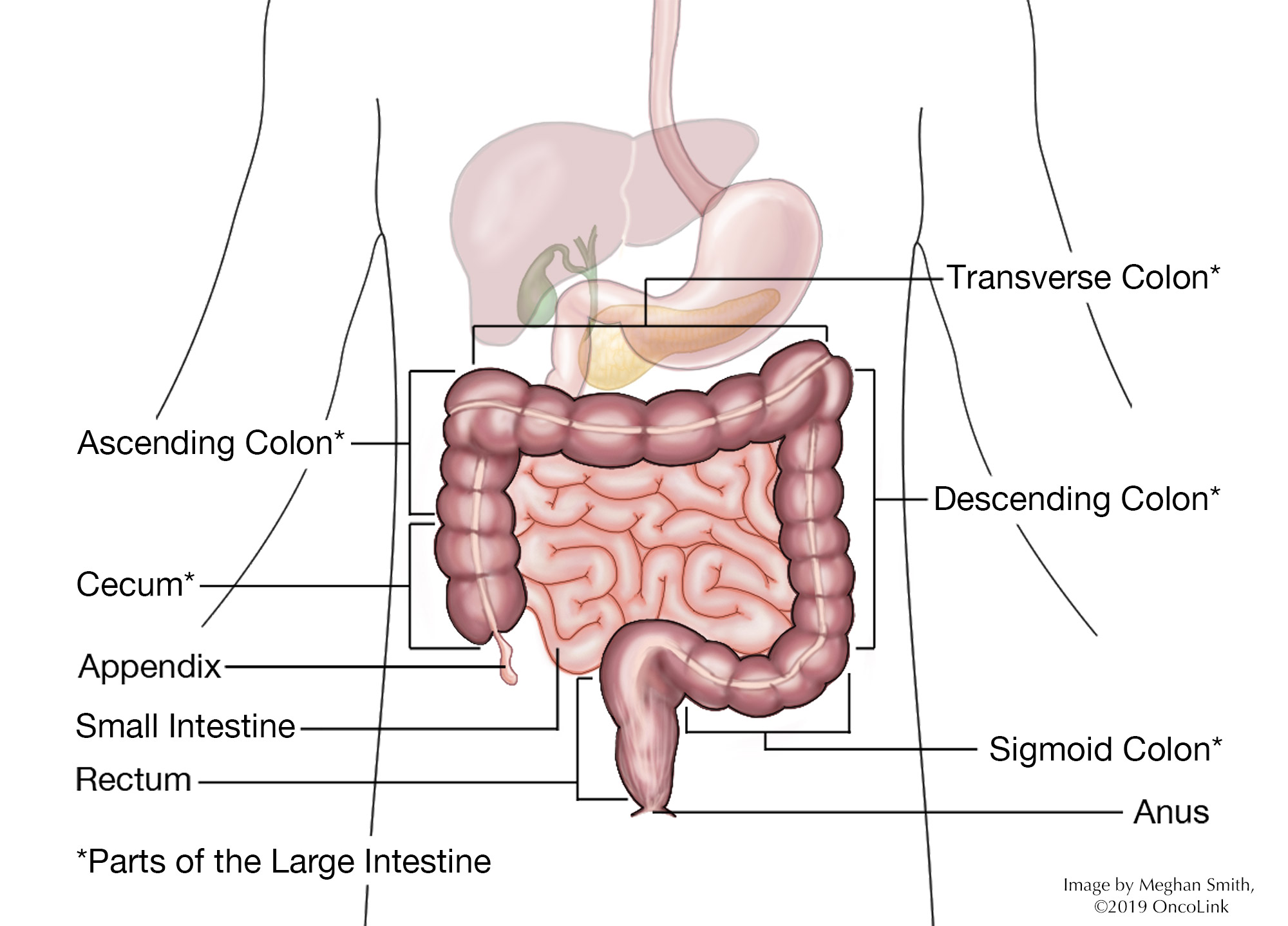
Your rectum is at the end of your colon. It is about 5 inches long. It is where stool (bodily waste) sits before it leaves your body. When there are cancer cells in the rectum, it is called rectal cancer.
Rectal cancer often starts in precancerous polyps. A polyp is a clump of cells that forms on the lining of your colon or rectum. Precancerous polyps are called adenomatous polyps. These polyps can turn into cancer and spread to the rectal wall. The most common type of rectal cancer is adenocarcinoma. Other types are:
What is staging and how is it done?
Staging is a way to find out if and where the cancer has spread in your body. Your provider will have you get a few tests to figure out the stage of your cancer. For rectal cancer, these tests may be:
Physical Exam: This is an exam to look at your body and to talk about past health issues.
Imaging: Radiology tests can look inside your body at the cancer and see if it has spread. These tests are:
- X-ray.
- CAT scan (CT scan).
- Positron emission tomography scan (PET scan).
- Magnetic resonance imaging (MRI).
- Endorectal/transrectal ultrasound.
Laboratory Testing: Blood tests such as blood chemistry and a complete blood count may be done. Other tests specific to testing for rectal cancer are:
- Fecal Occult Blood Testing: Also known as guaiac-based fecal occult blood test (gFOBT) and fecal immunochemical test (FIT). These test for blood in the stool.
- Stool DNA testing: This test looks for abnormal DNA found within the stool.
- Blood testing: Your care team may want to test levels of carcinoembryonic antigen (CEA) in your blood, which can be tested and tracked over time.
Procedures: Each case of rectal cancer is different. Talk with your care team about which procedures may be part of your treatment plan. These options may be:
- Colonoscopy: A colonoscope (lighted, flexible tube) is placed into the rectum to look at the whole colon and check for any changes or polyps. A biopsy may be done during this test.
- Sigmoidoscopy: A sigmoidoscope (lighted, flexible tube) is placed into the rectum and the lower part of the colon (called the sigmoid colon) to look for any changes. A biopsy may be done during this test.
- Double-contrast barium enema (Lower GI series): A liquid enema contrast, called barium, is put into your rectum. X-Rays are then taken to show any abnormalities of the lower gastrointestinal (GI) tract, including the colon and rectum.
- Biopsy: Biopsies may be taken to check for cancer. Your provider may also want to check for a genetic mutation called hereditary nonpolyposis colorectal cancer.
Rectal cancer spreads (metastasizes) to other parts of the body through the tissue, lymph, and blood systems. Cancer stage describes how extensive the cancer, how far it has spread and helps guide your treatment. Rectal cancer is described as stages 0 through stage IV (4) disease.
You will likely need surgery if you have rectal cancer.
Surgical Procedures for Rectal Cancer
There are a few surgical procedures used to treat rectal cancer, depending on your cancer stage and overall health, such as:
- Polypectomy/Local excision: A colonoscope (like with a colonoscopy) removes a polyp or an area of cancer. During a polypectomy, only the polyp is removed. During a local excision (also known as an endoscopic mucosal resection), some of the tissue on the rectal wall is also removed.
- Local transanal resection (Full thickness resection): The cancer is removed from the rectum, as well as some nearby healthy tissue through the anus. Some lymph nodes and the tissue between the rectum and abdominal (belly) wall may be removed. In some cases, the surgeon may use a magnifying scope to perform a transanal endoscopic microsurgery (TEM).
- Low anterior resection (LAR): The cancer is removed from the upper part of the rectum. Some healthy tissue and lymph nodes are also removed for testing. The colon and rectum are then re-connected. Sometimes a temporary ileostomy will be done to allow for healing.
- Abdominoperineal resection (APR): The anus, anal sphincter, and nearby tissue are removed. You will need a permanent (lifelong) colostomy.
- Proctectomy with colo-anal anastomosis: The whole rectum is removed, connecting the colon directly to the anus. At times, surgeons can connect a part of the rectum with a part of the colon that can store fecal matter to exit the body. In some cases, there is a need for a temporary (short-term) ileostomy.
- Radiofrequency ablation: Electrodes kill cancer through a probe placed through the skin or an abdominal incision.
- Cryosurgery: Abnormal cells are frozen and killed.
- Pelvic exenteration: Removes the rectum, bladder, and prostate in men or uterus in women. You will need a colostomy to remove stool and at times a urostomy to remove urine.
- Diverting colostomy: A rectal blockage can be relieved by placing a diverting colostomy (ostomy placed above the tumor in the GI tract).
- Surgery for metastatic disease: At times, rectal cancer may spread to other parts of the body, such as the lungs or liver, and it may need to be removed. These procedures depend on several factors that your healthcare provider will talk with you about.
Note: Your surgeon may consider minimally invasive surgery with laparoscopy or robotic surgery. There is also an option for nerve-preserving surgery, which aims to keep urinary and sexual function. Ask your provider which type of surgery is best for you.
What are the risks of rectal cancer surgery?
As with any surgical procedure, there are risks and side effects linked with rectal cancer surgery. These risks and side effects may be:
- Reaction to anesthesia (Anesthesia is the medication you are given to help you sleep through the surgery, to not remember it, and to manage pain).
- Bleeding.
- Blood clots.
- Infection.
- Anastomotic leak (leakage from the joined colon or anastomosis site).
- Pulling apart or splitting open of the incision.
- Adhesions/scar tissue.
- Bowel obstruction (blockage).
- Need for colostomy or ileostomy, which can affect body image.
- Possible erectile dysfunction (ED), orgasm changes, and impaired fertility in men.
- Possible painful intercourse and loss of ability to carry a child in women.
What is recovery like?
Recovery from rectal cancer surgery depends on the procedure that was done. A hospital stay is often needed.
You will be taught on how to care for your surgical incisions and/or ostomy and will be given any other instructions before leaving the hospital.
Your medical team will talk with you about the medications you will be taking, such as those for pain, blood clot, infection, constipation prevention and/or other conditions.
Your healthcare provider will go over any changes in your activity level depending on the surgery you have had. You will be given instructions on when to call your healthcare team.
What will I need at home?
- Thermometer to check for fever which can be a sign of infection. Your provider will tell you at what temperature you should call them.
- Loose clothes and underwear.
- Incision and/or ostomy care items, often supplied by the hospital/physician office.
How can I care for myself?
Depending on the type of surgery, you may need a family member or friend to help you with your daily tasks until you are feeling better and your care team tells you it is okay to resume normal activity.
Be sure to take your medications as directed to prevent pain, infection, or other conditions and call your medical team with any new symptoms.
If you have constipation, talk with your healthcare team about recommendations they have to offer relief.
Deep breathing and relaxation are important to help with pain, to keep lungs healthy after anesthesia, and to promote good drainage of lymphatic fluid. Try to perform deep breathing and relaxation exercises several times a day in the first week, or whenever you notice you are particularly tense.
- A simple exercise to do on your own: While sitting, close your eyes and take 5-10 slow deep breaths. Relax your muscles. Slowly roll your head and shoulders.
This hand-out provides general information only. Please be sure to discuss the specifics of your surgical plan and recovery with your surgeon.